-
All clinical experiences will be under the supervision of a qualified Registered Diagnostic Medical Sonographer, Registered Vascular Technologists or any other appropriately qualified registered ultrasound instructor.
-
Department assignments may direct the student to rotate in a particular setting or with a particular qualified instructor. This is designed to assist the student with registered instructors for optimal training and experiences.
-
According to our Standards, Operational Policies and the Diagnostic Medical Sonography Policies and Procedures supervision is defined as follows:
Direct Supervision
-
The qualified Registered Sonographer reviews the requisition of the examination and/or procedure in relation to the student’s achievement and the curriculum level completed.
-
The qualified Registered Sonographer evaluates the condition of the patient in relationship to the achievement and performance level of the student.
-
The qualified Registered Sonographer reviews and critiques ultrasound images with the student and approves all finished examinations.
-
After demonstrating competency, students may perform procedures with indirect supervision.
Indirect Supervision
-
Is supervision provided by a qualified Registered Sonographer who is immediately available to assist the student regardless of the level of the student’s achievement.
-
Immediately available is the presence of a qualified Sonographer adjacent to the room or location where an ultrasound examination is being performed.
Student Conduct
Diagnostic Medical Sonography Students are expected and required to conduct themselves in a professional manner at all times.
-
The DMS student must acknowledge the importance of the protection of confidential information concerning patients and their families. All personal information regarding a patient or his/her family is considered confidential. Any DMS student violating a patient’s right to confidentiality may be dismissed permanently from the DMS program upon proof of such violation.
-
The DMS student is required to follow all Baker College policies and procedures listed in the student handbook.
-
If the student is removed from the clinical site by Baker College or at the request of the clinical site, the student may be dismissed from the program.
-
The DMS student must park their cars in the designated area at their assigned clinical site.
Assignment of Duties
The clinical instructor will assist in making a schedule of student’s assignments in order for an orderly workflow and adequate rotation of practical clinical experience.
Specifically, the student will perform, to the best of his/her ability and accept any duty or task assigned by the clinical instructor. These tasks include but are not limited to transporting patients, gathering patient history, emptying dirty linens, and stocking scanning rooms. If there is a question in regards to this, please contact the Program Director, Clinical Coordinator or Clinical Instructor.
Daily clinical contact time is at the discretion of each specified clinical facility. Clinical instructors determine break times during the student’s assigned clinical day.
All Diagnostic Medical Sonography students will be under the supervision of a qualified sonographer. The assignment of clinical responsibilities increases, as the training period professes. All Diagnostic Medical Sonography students seeking employment to program completion will be advised to have completed all program clinical competencies. Any employment obtained prior to program completion, will not be counted as clinical time. All work hours should not interfere with program requirements and may not be substituted for the educational program clinical hours assigned.
Attendance of Clinical Experience
Full-time attendance is required in the classroom and in the clinical experience. The clinical experience is planned on a definite and scheduled basis. Each student will attend their clinical experience for 32 hours per week. Clinical assignments are in the best interest of the student to assure competency success for students.
Promptness for the classroom is an essential characteristic needed for advancement within the program. It is important that all assignments are completed on time and that students are properly prepared for class. These responsibilities are that of each individual student.
If a student is unable to be in class or attend their clinical experience, is it the student’s responsibility to notify the appropriate instructor. This notification needs to be done ASAP. If no notification is given, the appropriate program officials will be contacted. Not attending clinical requires a minimum of two contacts; Clinical Instructor at the assigned facility and the Baker College Clinical Coordinator.
Excused Absences From Clinical
Excused absence refers to time away from clinical, in which those hours do not need to be made up in a clinical setting prior to course completion.
-
One Sonography Conference (promoting continuing education), 8 clinical hours.
-
Approval of Conference is needed from the Program Director.
-
Proof of attendance must be returned to the Program Director
-
Cultural Diversity (example: Baker College Black History Month Expo), 8 clinical hours
-
All cultural diversity events must be approved by the Program Director.
-
Baker College Graduation
-
Summer Lab Assistance with New Students; 16 clinical hours.
-
Holidays specified by the Baker College System in which the campus is closed.
Program Policy Absenteeism, Tardiness, Dismissal and Leave of Absence
Absenteeism: Is defined as any loss of hours from the clinical setting. The student must notify the clinical affiliate and program official prior to the beginning of their shift. Failure to report absenteeism shall result in corrective action.
Excessive Absenteeism: Is defined as being absent more than two times in one semester. Excessive absenteeism will reflect on corrective action, probation and/or dismissal from the program at the discretion of the Dean of Health Sciences and Baker College Director of Sonography Programs.
Tardiness: Excessive Tardiness is unacceptable in the Diagnostic Medical Sonography Program, both for on ground courses and in the clinical setting. Sadly, this behavior can also result in dismissal from the clinical site and/or the Diagnostic Medical Sonography Program. Excessive Tardiness is defined as being tardy more than two times in one semester. Violations of any of these policies will result in corrective action; to include probation and or dismissal from the Diagnostic Medical Sonography Program.
Leave of Absence: Request for Leave of Absence is required for lost time of more than 3 consecutive days. Leave of absence may be granted only in exceptional circumstances (medial) and only by arrangements made with the Program Director. Proper documentation is required prior to returning to the program. All time missed for any reason, as listed above, shall be made up under the guidelines set by Baker College and an assigned clinical affiliate. This includes lost time due to inclement weather.
Bereavement Leave: A Diagnostic Medical sonography student who is absent from their clinical experience as a result of a death in their immediate family (or life network) shall, upon notification and approval of the clinical instructor, be entitled to a release time, not to exceed (3) scheduled days. The make-up policy for all lost clinical hours also applies to bereavement leave.
Federal Law Concerning Chemical Hazards
Federal law requires that all individuals must be notified about hazardous chemicals present in the workplace. This law applies to all occupations, with the basic purpose of raising the level of consciousness on chemical safety. Obviously, there are safe levels, proper procedures and precautions that must be followed when working with any chemicals.
Chemical supplies are required to prepare Material Safety Data Sheets (MSDS) for all chemicals in health care facilities, The MSDS sheets are available and accessible for review in student ultrasound labs. Once in a clinical setting, the clinical instructor can provide students with chemicals listed in their department.
Confidentiality of Student Records Policy
The Family Educational Rights and Privacy Act (FERPA) - See the Baker College Student Handbook; Official Records.
Infection Control Policy
Medical and surgical aseptic techniques are to be used while in the clinical setting to protect healthcare personnel, patients and students from transmission of potentially infectious organisms. Proper aseptic techniques will minimize the spread of infection, but it will not eliminate them. The following conditions are symptoms of possible infections and labeled reportable diseases. Students should not attend a clinical, if they have a reportable disease, until the condition is resolved. This may include any the following:
-
Diarrhea, vomiting, upper respiratory infection, fever, rash, open sores, boils, herpes, parasite infestation, strep or staph infection, infectious mononucleosis
Please see communicable disease policy.
Incident Reports
An incident is any happening, which is not consistent with the routine operation of the hospital or department, or the routine care of a particular patient. It may be an accident, a happening or a situation, which might result in an accident. Each affiliated clinical site will have its specific rules and regulations in reference to accidents, actions taken at the time of the reporting routine. These are made known to students during orientation period and shall be followed explicitly.
In addition to all requirements of reporting incidents in a clinical setting, a Baker College Incident form must all be completed. Baker College Incident Form Coming Soon!
Communicable Disease Policy
Objective: To protect health care personnel from transmission by considering ALL patients as potentially infected with HIV and/or other blood-borne pathogens and to adhere rigorously to infection control precautions for minimizing the risk of exposure to blood, body fluids and moist body substances of all patients.
-
All healthcare workers should routinely use appropriate barrier precautions to prevent skin and mucous-membrane exposure when contact with blood or other body fluids of any patient is anticipated. Gloves should be worn for touching blood and body fluids, mucous membranes or non-intact skin of all patients, for handling items or surfaces soiled with blood or body fluids and for performing venipuncture and other vascular access procedures. Gloves should be changed after contact with each patient. Masks and protective eyewear or face shields should be worn during procedures that are likely to generate droplets of blood or other body fluids to prevent exposure of mucous membranes of the mouth, nose and eyes. Gowns or aprons should be worn during procedures that are likely to generate splashes of blood or body fluids.
-
Hands and other skin surfaces should be washed immediately and thoroughly if contaminated with blood or other body fluids. Hands should routinely be washed immediately after gloves are removed.
-
All health-care workers should take precautions to prevent injuries caused by needles, scalpels and other sharp instruments or devices during procedures; when cleaning used instruments; during disposal of used needles and when handling sharp instruments after procedures. Refer to the procedure and policy manual of each clinical site for the specific methods for disposing of the objects mentioned above.
-
To provide a barrier during emergency mouth-to-mouth resuscitation, mouthpieces, resuscitation bags or other ventilation devices should be available for use in areas in which the need for resuscitation is predictable.
-
Healthcare workers who have exudative lesions or weeping dermatitis should refrain from all direct patient care and from handling patient care equipment until the condition resolves.
-
Pregnant healthcare workers are not known to be at greater risk of contracting HIV infection than healthcare workers who are not pregnant; however, if a healthcare worker develops HIV infections during pregnancy, the infant is at risk of infection resulting from prenatal transmission. Because of this risk, pregnant healthcare workers should be especially familiar with and strictly adhere to precautions to minimize the risk of HIV transmission.
-
Body fluids and substances such as feces, urine, airway secretions and wound drainage always contain potentially infectious organisms. Universal Precaution not only protects healthcare workers from transmission of blood-borne pathogens, but also from other infectious agents found in most body substances. Patients are protected from organisms present on the hands of personnel and the staff’s hands are protected from acquiring new organisms through proper hand-washing and wearing gloves.
Pregnancy Policy
Due to the importance of maintaining continual practice without interruption, students enrolled in the Diagnostic Medical Sonography program are strongly encouraged NOT to become pregnant during their clinical training. However, should a student have a confirmed pregnancy, they are encouraged to promptly inform the program director.
Upon confirmation of the pregnancy, the student will:
-
Submit a “Notice of Pregnancy” form to the Diagnostic Medical Sonography Program Director.
-
Submit a statement from her physician verifying pregnancy and expected due date. The statement must include the physician’s recommendation of the following options:
-
Student’s status remains unchanged.
-
Withdrawal from the clinical component of the program.
-
A modification of clinical responsibilities.
-
Submit in writing within two days the student’s decision concerning the recommendations of the student’s physician.
-
A leave of absence, not recommended by the physician, will be reviewed on an individual basis by the program director and clinical coordinator.
-
If the pregnant student remains in the Diagnostic Medical Sonography program, the student will be required to abide by the following:
-
Strict adherence to all safety precautions for protection purposes.
-
The student must notify the program director and clinical coordinator of any change in health status during the pregnancy that may affect clinical performance.
-
If at any time the pregnant student feels she is working in an unsafe area or under unsafe conditions, the student must stop immediately and report to the clinical instructor.
-
If the pregnant student withdraws from the Diagnostic Medical Sonography program because of pregnancy during the second year of the program, re-admittance will be under the following conditions:
-
The student was in “good standing” academically at the time of withdrawal.
-
The student may be able to return to the program after receipt of a medical release from the student’s physician.
-
The student will be expected to complete the clinical component of the program to document the hours needed for clinical practice. If necessary, this may require the student to attend beyond the date that the program would have ended.
-
The student may need to wait until the following year to re-enter the program because courses are offered only once per year and clinical practice coincides with classroom material.
Curriculum Design - Sequencing of Courses
Assessment and Competencies
Required with the 1504 hours of clinical are 11 assessments and 9 competencies.
Clinical Hours
In the DMS Program, the clinical experience includes 3 clinical semester courses. During clinical rotation, the student will complete a total of 1504 clinical hours. Holidays that are observed during the clinical rotation: Labor Day, Thanksgiving, New Year’s Day, MLK Day, Memorial Day, and 4th of July.
Fall Semester: 536 clinical hours.
Spring Semester: 568 clinical hours
Summer Semester: 400 clinical hours
Total: 1504 clinical hours
HEALTH INFORMATION MANAGEMENT
Program Overview
A Health Information Management professional is skilled and responsible for maintaining, organizing, and producing medical information. The curriculum prepares students for employment in any healthcare setting. Upon completion of the program, graduates are eligible to sit for the RHIA National Certification Exam.
Accreditation Information
The Baccalaureate Degree Program in Health Information Management at Baker College Online is accredited by the Higher Learning Commission (HLC).
State and National Organizations (Membership)
The HIT Program requires mandatory student membership in AHIMA/MHIMA. The annual cost is $49.00.
Goals
-
The primary goal of the Health Information Management Program at Baker College is to establish and maintain an educational program of the highest quality.
-
It is our intent to graduate students who have developed the professional and personal attitude and skills necessary to begin their careers as health information technicians and successfully pass the national examination.
-
To achieve this goal, an appropriate curriculum has been developed for the Health Information Management Program, which enables the student to demonstrate the Domains for health information administrator.
Mission
The Mission of the Health Information Management program is to provide students with the opportunity to build on knowledge and develop the skills necessary to be employed as a Health Information Management professional.
Program Outcomes/Philosophy
-
Apply health information management skills such as data analysis, abstracting, coding validation, reimbursement methodologies, retrieval, and quality measurement of healthcare data to the work environment.
-
Demonstrate written and verbal organizational skills to facilitate team meetings that support a culture of diversity within the healthcare environment.
-
Communicate using the oral and written communication skills necessary for effective interaction with multidisciplinary teams, providers, and consumers in the healthcare work environment.
-
Apply critical thinking skills to effectively solve health information management problems.
-
Apply ethical decision-making as it pertains to HIPAA, confidentiality, and privacy.
-
Analyze policies and procedures to ensure organizational compliance with regulations and standards.
Program Learning Objectives
The Health Information Management (HIM) profession includes managers, technicians and special experts in HIM systems and processes. Upon completion of the Health Information Management Program, the graduate shall demonstrate the following entry-level competencies as identified by the American Health Information Management Association Council for Excellence in Education:
Domain I: Data Structure, Content, and Information Governance
-
Compare diverse stakeholder perspectives through the delivery of health care services.
-
Analyze strategies for the management of information.
-
Evaluate policies and strategies to achieve data integrity.
-
Recommend compliance of health record content across the system.
-
Utilize classification systems, clinical vocabularies, and nomenclatures.
-
Evaluate data dictionaries and data sets for compliance with governance standards.
Domain II: Information Protection: Access, Uses, Disclosure, Privacy and Security
-
Recommend privacy strategies for health information.
-
Recommend security strategies for health information.
-
Analyze compliance requirements throughout the health information life cycle.
Domain III: Informatics, Analytics and Data Use
-
Examine health informatics concepts for the management of health information.
-
Analyze technologies for health information management.
-
Interpret statistics for health care operations.
-
Examine health care findings with data visualizations.
-
Compare research methodologies pertaining to health care.
-
Manage data within a database management system.
-
Identify standards for the exchange of health information.
Domain IV: Revenue Cycle Management
-
Evaluate assignment of diagnostic and procedural codes and groupings in accordance with official guidelines.
-
Manage components of the revenue cycle.
-
Evaluate compliance with regulatory requirements and reimbursement methodologies.
Domain V: Health Law and Compliance
-
Comply with legal processes impacting health information.
-
Evaluate compliance with external forces.
-
Analyze components of risk management related to health information management.
-
Analyze the impact of policy on health care.
Domain VI: Organizational Management and Leadership
-
Facilitate fundamental leadership skills.
-
Assess the impact of organizational change.
-
Analyze human resource strategies for organizational best practices.
-
Leverage data-driven performance improvement techniques for decision making.
-
Verify financial management processes.
-
Examine behaviors that embrace cultural diversity.
-
Assess ethical standards of practice.
-
Facilitate consumer engagement activities.
-
Facilitate training needs for a health care organization.
-
Compare project management methodologies to meet intended outcomes.
Description of the Profession
The Health Information Management program is designed to provide a solid foundation in healthcare organization operations, including healthcare regulation, project management of health systems, computer information systems, database privacy, and security of health information. The program prepares students in the health information department of clinics and hospitals to manage and oversee data, information technology, healthcare compliance, revenue and coding, privacy, security, and medical record operations.
Code of Ethics
Health Requirements
Evidence of acceptable health status prior to beginning the PPE is required for all students. The evidence must be given to the PPE Clinical Coordinator who will maintain the form in the student’s file. Evidence will be in the form of a TB test with a documented negative reading by a qualified healthcare professional. Students will not be permitted to begin the PPE without this evidence. Any student who declines the TB test may be ineligible for PPE placement in certain facilities.
The PPE site may require additional immunizations for the student as a condition of the PPE. Any student who declines requested immunizations will be ineligible for PPE placement.
Curriculum
A Baccalaureate Science degree with a major in Health Information Management is granted by the College after completion of the course requirements in the four-year program. The student will be required to successfully complete all courses listed on the Degree Audit.
A minimum grade of “B-” must be earned in each HIT and HIM course and a minimum grade of “C” must be earned in BIO1210, BIO1211, and BIO1250. In order to enroll for the Professional Practice Experience (PPE) course HIM4350, the student must have successfully completed all courses with an overall grade point average of at least 2.5. Students not receiving at least a B- in the required HIT and HIM courses will not be allowed to continue onto the next sequential HIT or HIM course. Students may also be placed on Academic Probation when not achieving a B- in a HIT or HIM course. Students must repeat the identified HIT or HIM course with at least a B- before being placed into a professional practice experience.
Professional Requirements and Technical Skills
These technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the program at Baker College. These standards are not conditions of admission to the program. Persons interested in applying for admission to the program should review this information to develop a better understanding of the physical abilities and behavioral characteristics necessary to successfully complete the program. The College complies with the requirements and Section 504 of the Rehabilitation Act and the Americans with Disabilities Act of 1990. Therefore, the College will endeavor to provide reasonable accommodation for participants with disabilities who are otherwise qualified.
-
Access to information from books, reference manuals, computers and paper and electronic medical records to accurately perform HIM functions and duties.
-
Utilize electronic equipment and medical records.
-
Correctly interpret and/or clarify verbal, written and electronic health information.
-
Prioritize, organize, and disseminate accurate health information.
-
Safely access and operate equipment in a variety of settings.
-
Demonstrate professional and procedural judgment under stressful, emergent and/or a distracting environment (1.3., high noise levels, crowding and complex sensory stimuli).
-
Adhere to HIPAA, AHIMA (American Health Information Management Association) professional standards Baker College and clinical site PPE guidelines.
Supervision Requirements
All professional practice experiences will be under the supervision of a qualified professional to reinforce didactic instruction and must include program-coordinated experience at professional practice sites.
Clinical Hours
Health Information Management sites are open Monday through Friday. The start and end times will vary by facility availability and staffing needs. Students currently employed in the healthcare field may desire to complete their PPE with their existing employer. In this circumstance, the student must complete their 120 PPE hours in a different department or perform functions that are not part of their regular employment responsibilities. Students will begin the PPE in the second 8 weeks of the spring 2 semester and not later than six (6) months after completion of the HIM program.
During the fall semester of the last year of study, the student will meet with the PPE Clinical Coordinator to review the rules and student responsibilities during the PPE, as well as project requirements. The Clinical Coordinator will then place the student in a PPE site and notify the student.
Miscellaneous Information Regarding Profession Practice Experience (PPE) Externships
-
Students are encouraged to contact facilities regarding potential PPE placement. The Program Director/Clinical Coordinator retains the responsibility for obtaining required legal agreements and assessing the site’s appropriateness for individual student needs.
-
Most sites specify that a student must interview in person prior to acceptance.
-
If sites have additional requirements (specific immunizations, additional background checks, drug screening or fingerprinting) students are responsible for any and all costs associated with these site requirements.
-
Any site has the option of not taking a student due to staffing issues, etc.
-
Students may receive assignments that are far away, and students are required to provide their own transportation and/or lodging to fulfill their PPE requirements.
-
All placement decisions are at the discretion of the PPE Clinical Coordinator.
-
The student may not be paid for any part of the PPE hours.
-
Two background checks will be conducted on every student. The first background check will occur Spring 1 semester. The second background check will occur during Fall 2 semester. The student will be responsible for the costs of background check(s). A criminal record may prevent clinical affiliation site placement and or employment opportunities. The student is required to complete and submit the background check results to the Program Director by the deadline specified. Baker College reserves the right to deny entry into or remove from a program any student whose background check reveals any felony conviction or recorded event of any nature. The student will immediately report, in writing, any conviction pending court action or other recorded event that has not yet been reported or that subsequently occurs to the Program Director.
-
Prior to the beginning of the Professional Practice Experience (PPE), the student will disclose the background check results to the clinical coordinator/or Program Director. When deemed necessary, the clinical coordinator and student will schedule a face-to face meeting with the clinical site supervisor to discuss the nature of the background check.
-
Once a PPE placement is made, should the student refuse or need to cancel the assigned placement, the student must wait until another site becomes available. Due to limited affiliation sites, this potentially may defer the postponement
-
The student has 6 months from the date of completion of the last HIM course to complete the PPE or will need to apply for reentry into the program.
-
PPE Self Placement Process - Please see HIM OL PPE Procedure HIM PPE Procedure Form Coming Soon!
Professionalism
Students are expected to demonstrate professional behavior within classes and during the externship experience that reflects the seriousness and dedication required of a professional in the medical field. These behaviors will include but are not limited to verbal and nonverbal language, mannerisms, preparedness, dress, attitude, cooperation, confidentiality, caring personality, willingness to help others and flexibility. Students not meeting these criteria will be subject to dismissal from the program.
National Certification Exam
The National Registered Health Information Technology (RHIT) Certification Examination is administered by a professional examination service for the American Health Information Management Association (AHIMA). Successful completion of this examination permits the individual to use the credentials “RHIT” or “Registered Health Information Technician.”
Students are eligible to sit for the RHIT credentialing examination.
Completion of all graduation requirements will enable the student to sit for the National Certification Examination. Upon application approval, the eligibility period for taking the exam is four (4) months. The exam is in an online format and available to the student with an appointment. Applications and exam information is available on the
AHIMA website and will be discussed in the program capstone course HIM4310, RHIA Review.
Curriculum Design - Sequencing of Courses
See Program Website
HEALTH INFORMATION TECHNOLOGY
Program Overview
A Health Information Technician is a skilled professional responsible for maintaining, organizing, and producing medical information. The curriculum prepares students for employment in any healthcare setting. Upon completion of the program, graduates are eligible to sit for the RHIT National Certification Exam.
Accreditation Information
The Associate Degree Program in Health Information Technology at Baker College Online is accredited by the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM).
State and National Organizations (Membership)
The HIT Program requires mandatory student membership in AHIMA/MHIMA. The annual cost is $49.00.
Goals
-
The primary goal of the Health Information Technology Program at Baker College is to establish and maintain an educational program of the highest quality.
-
It is our intent to graduate students who have developed the professional and personal attitude and skills necessary to begin their careers as health information technicians and successfully pass the national examination.
-
To achieve this goal, an appropriate curriculum has been developed for the Health Information Technology Program, which enables the student to demonstrate the Domains for health information technicians.
Mission
The Mission of the Health Information Technology program is to provide students with the opportunity to build on knowledge and develop the skills necessary to be employed as a Health Information Management professional.
Program Outcomes
-
Apply health information management skills such as data analysis, abstracting, coding validation, reimbursement methodologies, retrieval, and quality measurement of healthcare data to the work environment.
-
Demonstrate written and verbal organizational skills to facilitate team meetings that support a culture of diversity within the healthcare environment.
-
Communicate using the oral and written communication skills necessary for effective interaction with multidisciplinary teams, providers, and consumers in the healthcare work environment.
-
Apply critical thinking skills to effectively solve health information management problems.
-
Apply ethical decision-making as it pertains to HIPAA, confidentiality, and privacy.
-
Analyze policies and procedures to ensure organizational compliance with regulations and standards.
Philosophy
Curriculum is a dynamic process, creating a dialogue between faculty and students that encourages a shared responsibility for learning. Although the acquisition of content knowledge and technical skills are expected outcomes, the focus is on the development of critical thinking skills, personal growth, professional development, and awareness of global issues essential for lifelong learning. It recognizes that learning occurs in the online classroom, with students and faculty challenged to question, analyze, problem-solve and to be open and accepting of differing views.
Program Learning Objectives
The Health Information Management (HIM) profession includes managers, technicians and special experts in HIM systems and processes.
Upon completion of the Health Information Technology Program, the graduate shall demonstrate the following entry-level competencies as identified by the American Health Information Management Association Council for Excellence in Education:
Domain I: Data Structure, Content, and Information Governance
-
Describe health care organizations from the perspective of key stakeholders.
-
Apply policies, regulations, and standards to the management of information.
-
Identify policies and strategies to achieve data integrity.
-
Determine Compliance of health record content within the health organization.
-
Explain the use of classification systems, clinical vocabularies, and nomenclatures.
-
Describe components of data dictionaries and data sets.
Domain II: Information Protection: Access, Uses, Disclosure, Privacy and Security
-
Apply privacy strategies to health information.
-
Apply security strategies to health information.
-
Identify compliance requirements throughout the health information life cycle.
Domain III: Informatics, Analytics and Data Use
-
Apply health informatics concepts to the management of health information.
-
Utilize technologies for health information management.
-
Calculate statistics for health care operations.
-
Report health care data through graphical representations.
-
Describe research methodologies used in health care.
-
Describe the concepts of managing data.
-
Summarize standards for the exchange of health information.
Domain IV: Revenue Cycle Management
-
Validate assignment of diagnostic and procedural codes and groupings in accordance with official guidelines.
-
Describe components of revenue cycle management and clinical documentation improvement.
-
Summarize regulatory requirements and reimbursement methodologies.
-
RM Determine diagnosis and procedure codes according to official guidelines.
-
RM Evaluate revenue cycle processes.
-
RM Evaluate compliance with regulatory requirements and reimbursement methodologies.
Domain V: Health Law and Compliance
-
Apply legal processes impacting health information.
-
Demonstrate compliance with external forces.
-
Identify the components of risk management related to health information management.
-
Identify the impact of policy on health care.
Domain VI: Organizational Management and Leadership
-
Demonstrate fundamental leadership skills.
-
Identify the impact of organizational change.
-
Identify human resource strategies for organizational best practices.
-
Utilize data-driven performance improvement techniques for decision making.
-
Utilize financial management processes.
-
Examine behaviors that embrace cultural diversity.
-
Assess ethical standards of practice.
-
Describe consumer engagement activities.
-
Identify processes of workforce training for health care organizations.
Description of the Profession
The health information technician possesses the technical knowledge and skills necessary to maintain components of health record systems consistent with the requirements of the healthcare delivery system. In all types of healthcare facilities and in various locations within a facility, the health information technician analyzes health records according to standards; abstracts and codes diagnoses and procedures; maintains and utilizes a variety of health record indexes and registries; and compiles administrative and health statistics and prepares reports for reimbursement, facility planning, marketing, quality assessment and research.
Code of Ethics
Health Requirements
All health science students are required to have the COVID-19 vaccination.
Evidence of acceptable health status prior to beginning the PPE is required for all students. The evidence must be given to the PPE Clinical Coordinator who will maintain the form in the student’s file. Evidence will be in the form of a TB test with a documented negative reading by a qualified healthcare professional. Students will not be permitted to begin the PPE without this evidence. Any student who declines the TB test may be ineligible for PPE placement in certain facilities.
The PPE site may require additional immunizations for the student as a condition of the PPE. Any student who declines requested immunizations will be ineligible for PPE placement.
Curriculum
An Associate of Applied Science degree with a major in Health Information Technology is granted by the College after completion of the course requirements in the two-year program. The student will be required to successfully complete all courses listed on the Degree Audit.
A minimum grade of “B-” must be earned in each HIT course and a minimum grade of “C” must be earned in BIO1210, BIO1211, HSC1250. In order to enroll for the Professional Practice Experience (PPE) course HIT2510, the student must have successfully completed all courses with an overall grade point average of at least 2.5. Students not receiving at least a B- in the required HIT courses will not be allowed to continue onto the next sequential HIT course. Students may also be placed on Academic Probation when not achieving a B- in a HIT course. Students must repeat the identified HIT course with at least a B- before being placed into a professional practice experience.
Professional Requirements and Technical Skills
These technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the program at Baker College. These standards are not conditions of admission to the program. Persons interested in applying for admission to the program should review this information to develop a better understanding of the physical abilities and behavioral characteristics necessary to successfully complete the program. The College complies with the requirements and Section 504 of the Rehabilitation Act and the Americans with Disabilities Act of 1990. Therefore, the College will endeavor to provide reasonable accommodation for participants with disabilities who are otherwise qualified.
-
Access to information from books, reference manuals, computers and paper and electronic medical records to accurately perform HIM functions and duties.
-
Utilize electronic equipment and medical records.
-
Correctly interpret and/or clarify verbal, written and electronic health information.
-
Prioritize, organize, and disseminate accurate health information.
-
Safely access and operate equipment in a variety of settings.
-
Demonstrate professional and procedural judgment under stressful, emergent and/or a distracting environment (1.3., high noise levels, crowding and complex sensory stimuli).
-
Adhere to HIPAA, AHIMA (American Health Information Management Association) professional standards Baker College and clinical site PPE guidelines.
Supervision Requirements
All professional practice experiences will be under the supervision of a qualified professional to reinforce didactic instruction and must include program-coordinated experience at professional practice sites.
Clinical Hours
Health Information Technology sites are open Monday through Friday. The start and end times will vary by facility availability and staffing needs. Students currently employed in the healthcare field may desire to complete their PPE with their existing employer. In this circumstance, the student must complete their 120 PPE hours in a different department or perform functions that are not part of their regular employment responsibilities. Students will begin the PPE in the second 8 weeks of the spring 2 semester and not later than six (6) months after completion of the HIT program.
During the fall semester of the last year of study, the student will meet with the PPE Clinical Coordinator to review the rules and student responsibilities during the PPE, as well as project requirements. The Clinical Coordinator will then place the student in a PPE site and notify the student.
Miscellaneous Information Regarding Profession Practice Experience (PPE) Externships
-
Students are encouraged to contact facilities regarding potential PPE placement. The Program Director/Clinical Coordinator retains the responsibility for obtaining required legal agreements and assessing the site’s appropriateness for individual student needs.
-
Most sites specify that a student must interview in person prior to acceptance.
-
If sites have additional requirements (specific immunizations, additional background checks, drug screening or fingerprinting) students are responsible for any and all costs associated with these site requirements.
-
Any site has the option of not taking a student due to staffing issues, etc.
-
Students may receive assignments that are far away, and students are required to provide their own transportation and/or lodging to fulfill their PPE requirements.
-
All placement decisions are at the discretion of the PPE Clinical Coordinator.
-
The student may not be paid for any part of the PPE hours.
-
Two background checks will be conducted on every student. The first background check will occur Spring 1 semester. The second background check will occur during Fall 2 semester. The student will be responsible for the costs of background check(s). A criminal record may prevent clinical affiliation site placement and or employment opportunities. The student is required to complete and submit the background check results to the Program Director by the deadline specified. Baker College reserves the right to deny entry into or remove from a program any student whose background check reveals any felony conviction or recorded event of any nature. The student will immediately report, in writing, any conviction pending court action or other recorded event that has not yet been reported or that subsequently occurs to the Program Director.
-
Prior to the beginning of the Professional Practice Experience (PPE), the student will disclose the background check results to the clinical coordinator/or Program Director. When deemed necessary, the clinical coordinator and student will schedule a face-to face meeting with the clinical site supervisor to discuss the nature of the background check.
-
Once a PPE placement is made, should the student refuse or need to cancel the assigned placement, the student must wait until another site becomes available. Due to limited affiliation sites, this potentially may defer the postponement
-
The student has 6 months from the date of completion of the last HIT course to complete the PPE or will need to apply for reentry into the program.
-
PPE Self Placement Process HIT PPE Procedure Form Coming Soon!
Professionalism
Students are expected to demonstrate professional behavior within classes and during the externship experience that reflects the seriousness and dedication required of a professional in the medical field. These behaviors will include but are not limited to: verbal and nonverbal language, mannerisms, preparedness, dress, attitude, cooperation, confidentiality, caring personality, willingness to help others and flexibility. Students not meeting these criteria will be subject to dismissal from the program.
National Certification Examination
The National Registered Health Information Technology (RHIT) Certification Examination is administered by a professional examination service for the American Health Information Management Association (AHIMA). Successful completion of this examination permits the individual to use the credentials “RHIT” or “Registered Health Information Technician.”
Students are eligible to sit for the RHIT credentialing examination.
Completion of all graduation requirements will enable the student to sit for the National Certification Examination. Upon application approval, the eligibility period for taking the exam is four (4) months. The exam is in an online format and available to the student with an appointment. Applications and exam information is available on the
AHIMA website and will be discussed in the program capstone course HIT2910, RHIT Review.
Curriculum Design - Sequencing of Courses
Health Information Technology Academic Plan
Medical Assistant
Program Overview
The Medical Assistant program is a 2-semester 30 credit hour certificate degree. Medical assisting is a multi-skilled allied healthcare profession in which practitioners work primarily in ambulatory settings such as medical offices and clinics. Medical assistant’s function as members of the healthcare delivery team and perform administrative duties and clinical procedures. Graduates are encouraged to take the American Association of Medical Assistants (AAMA) national certifying exam. Passing this exam entitles the candidate to the credential Certified Medical Assistant (CMA).
Accreditation Information
The Medical Assistant Program is at the Cadillac campus and is accredited by the:
Commission on Accreditation of Allied Health Education Programs (CAAHEP)
9355 113th St. N, #7709, Seminole, FL 33775
Phone: (727) 210-2350
CAAHEP accredits the program based upon the recommendation of the:
Medical Assisting Education Review Board (MAERB)
2339 N. California Ave, #47138, Chicago, IL 60647
Phone: (312) 392-0155
National Organizations (Membership)
American Association of Medical Assistants (AAMA) 20 N Wacker Drive, Suite 1575
Chicago, IL 60606
Phone: 312-899-1500
Students are encouraged to become student members of the American Association of Medical Assistants (AAMA). Students are encouraged to affiliate with their local chapter of the AAMA. Please see resources below or contact the medical assisting program director at your campus for this information. Michigan Society of Medical Assistants
http://www.MSMAonline.org Local chapters for the state of Michigan are listed on the MSMA website.
Mission
The mission of Baker College’s Medical Assistant Program is to prepare medical assistants who are competent in the cognitive (knowledge), psychomotor (skills), and affective (behavior) learning domains to enter the profession. Students will gain the core knowledge and skills needed to provide professional care while performing administrative and clinical tasks in a healthcare setting.
Program Goals
The goal of this Medical Assistant Program is to provide the healthcare community a multi- skilled healthcare professional specifically educated to work in ambulatory settings performing administrative and clinical duties. The practice of medical assisting has a profound influence on the health and wellbeing of the community and requires mastery level knowledge and skills obtained by both a formal education and a practical experience. In addition, the Medical Assistant program at Baker College prepares its graduates to participate and pass a National Certification exam. These goals will be accomplished by meeting the essentials as well as the standards and guidelines adopted by and set forth by the Commission on Accreditation of Allied Health Education Programs (CAAHEP), the American Association of Medical Assistants (AAMA).
-
Perform administrative skills required of an entry-level medical assistant. This includes EHRs, basic finance concepts, effective communication, cultural diversity, appointment scheduling, third party reimbursement and billing and coding procedures.
-
Demonstrate competency in the clinical skills of an entry-level medical assistant including, mathematics in patient care, infection control, protective practices, CLIA waived testing, venipuncture and first aid.
-
Identify legal concepts and ethical considerations specific to the healthcare setting.
-
Prepare to sit for the national credentialing exam.
Code of Ethics
The Medical Assisting Code of Ethics of the AAMA sets forth principles of ethical and moral conduct as they relate to the medical profession and the particular practice of medical assisting.
Members of the AAMA dedicated to the conscientious pursuit of their profession and thus desiring to merit the high regard of the entire medical profession and the respect of the general public which they serve, do pledge themselves to strive always to:
-
Render service with full respect for the dignity of humanity.
-
Respect confidential information obtained through employment unless legally authorized or required by responsible performance of duty to divulge such information.
-
Uphold the honor and high principles of the profession and accept its disciplines.
-
Seek to continually improve the knowledge and skills of medical assistants for the benefit of patients and professional colleagues.
-
Participate in additional service activities aimed toward improving the health and well-being of the community.
Safety Requirements
Laboratory and Blood Borne Pathogens training are required in MA 1010. Pregnant students enrolled in MA 1410 are encouraged to have a doctor’s release in order to participate in invasive procedures.
Occupational Risks
Medical Assisting is a profession with many rewards, as practitioners can perform both administrative and clinical services, filling several roles in a variety of healthcare environments. The Bureau of Labor Statistics clearly outlines that it is a growth field, with an anticipated 18% growth from 2020 to 2030.
Medical Assistants work directly with providers and patients, with the goal of providing healthcare and ensuring patient safety. It is a position with a great deal of responsibility.
As with any healthcare position, there are certain occupational risks that come into play with being a medical assistant, and those hazards include the following:
- Exposure to infectious diseases
- Sharps injuries
- Bloodborne pathogens and biological hazards
- Chemical and drug exposure
- Ergonomic hazards from lifting, sitting, and repetitive tasks
- Latex allergies
- Stress
At the same time, there are protections set up with the Occupational Safety and Health Act (OSHA), and those protections are particularly important within a healthcare environment. OSHA has a series of standards that protect the safety of healthcare workers and patients.
Accredited medical assisting programs are required to teach students about the hazards that they face on the job and the protocols that can be put into place to ensure a workplace culture that prioritizes safety. This content will be discussed in MA 1010 Basic Clinical and Administrative Skills.
Transfer Policy
The Baker College program director reserves the right to test any student transferring from a program that is an accredited program to evaluate and document evidence the student has met the cognitive, psychomotor and affective learning domains of the program students. Students are responsible for any associated costs or fees for testing and evaluation. Baker College will not accept transfer credits from non-accredited medical assisting programs.
Professional Requirements and Technical Skills
Technical skills must be met with or without accommodations. A student seeking admission into the medical assisting program at Baker College should carefully review these non- academic technical standards and decide if the perspective students has any limitations that may restrict or interfere with the satisfactory performance of any of these requirements.
Minimum acceptable mental and physical qualifications of an applicant for professional medical assistant include the following abilities:
-
Frequently work in a standing position and do frequent walking.
-
Lift and transfer patients up to (6”) from a stooped position, then push or pull the weight up to three feet (3’).
-
Lift and transfer patients from a stooped to an upright position to accomplish exam table- to-chair and chair-to-exam table.
-
Physically apply up to ten pounds (10#) of pressure to bleeding sites or in performing CPR.
-
Respond and react immediately to verbal instructions/requests and to auditory signals from monitoring equipment; perform auditory auscultation without impediment.
-
Physically perform up to a twelve-hour shift clinical laboratory experience.
-
Physically close and distance visual activities involving objects, persons, and paperwork, as well as discriminate depth and color perception.
-
Discriminate between sharp/dull and hot/cold when u sing both hands.
-
Perform mathematical calculations for medication preparation and administration.
-
Communicate effectively, both orally and in writing, using appropriate grammar, vocabulary, work usage and interpersonal skills.
Uniform Dress Code
-
Full uniform includes a top, pants and athletic shoes. Uniforms should be properly maintained. Program directors will provide specific color for your campus.
-
Hair that is shoulder length or longer must be pulled back during clinical labs.
-
Students are required to obtain/maintain Provider level CPR and First Aid certification and provide proof of it to the program director.
Supervision Requirements
On-site supervision of the student during practicum must be provided by an individual who has knowledge of the medical assisting profession.
Credential Requirements
-
Students in an accredited program are eligible to sit for the Certified Medical Assistant (CMA) credential through the American Association of Medical Assistants (AAMA) upon successful completion of the Certificate Program in Medical Assisting. The professional credentialing agency Web site is as follows:
www.aama-ntl.org.
-
The AAMA Disciplinary Standards and Procedures for CMAs (AAMA) and Exam Candidates states: If you were found guilty or a felony, or pleaded guilty to a felony, it could be grounds for denial of eligibility for the CMA (AAMA) credential.
-
Other credentialing opportunities are available for the MA graduate. See program director for details.
Curriculum Design - Sequencing of Courses
Degree Completion Requirements
Students are required to successfully pass all major courses listed in the Baker College Catalog with a C (73%) or better. No substitutions or experiential credit may be granted for MA courses.
Competencies
The program must demonstrate that the content and competencies included in the program’s curriculum meet or exceed those stated in the MAERB Core Curriculum. The full list of core competencies can be found here in appendix B.
Clinical Hours
Students are required to complete a 160-hour work experience. Students must successfully complete all core MA classes with a C or better to be placed into a practicum. It is extremely important that the student begin their practicum within a reasonable time, following the completion of their didactic work. Approval from the program coordinator/director is required prior to registration for the practicum. MAERB Policy #145: At the healthcare practicum site, the students must be supervised, cannot be substituted for staff and must be readily identifiable as students.
Clinical site placement will be assigned by the program coordinator/director. Students who refuse a clinical site placement will not be reassigned. Students shall not place themselves for their clinical experience. Baker College is not obligated to reassign students a clinical site, once rejected from a site for attendance issues, unprofessional conduct or any other circumstance as documented by the program coordinator/director and/or site.
Placement at the practicum site is by program official assignment and is based on availability, location, site supervisor preference etc. Practicum sites are selected to give the student the best overall experience. The student is expected to perform both administrative and clinical duties.
OCCUPATIONAL THERAPY ASSISTANT
Program Overview
Occupational therapy assistants, working under the supervision of occupational therapists, provide skilled treatments to individuals across the lifespan. Treatment interventions are designed to promote successful engagement in everyday activities (occupations). These include the skills necessary for learning, social interaction and recovery from emotional, physical or cognitive limitations. A felony conviction may affect a graduate’s ability to sit for the NBCOT examination or attain state licensure.
Accreditation Information
The Occupational Therapy Assistant Programs at Baker College of Owosso and Muskegon are fully accredited by:
Accreditation Council for Occupational Therapy Education (ACOTE)
7501 Wisconsin Avenue, Suite 510E, Bethesda, MD 20814
Phone: (301) 652-6611
www.acoteonline.org
Graduates are eligible to take the national certification examination.
State and National Organizations
- The American Occupational Therapy Association (AOTA)
- The Michigan Occupational Therapy Association (MiOTA)
Mission
The mission of the Occupational Therapy Assistant Program at Baker College is to prepare skilled, compassionate, and competent entry-level occupational therapy assistants who are eligible to sit for the national certification and ready to meet the demands of the healthcare industry.
OTA Program Core Values
The faculty of the Occupational Therapy Program support the mission, vision and core values of Baker College.
Integrity: Faculty will maintain honesty, transparency, and trustworthiness in all professional interactions and decisions.
Caring: As faculty, we emphasize the importance of teaching OTAs to deliver client-centered care grounded in empathy and compassion. Our curriculum is designed to develop students’ ability to build therapeutic relationships, understanding that caring is integral to effective intervention.
Inclusiveness: As faculty, we are committed to fostering an inclusive learning environment that reflects the diverse populations our students will serve. Our program emphasizes the development of cultural awareness and sensitivity, ensuring that future OTAs are prepared to provide equitable care.
Innovation: As faculty, we foster creativity, flexibility, and inspire critical thinking in therapeutic approaches, preparing students to integrate innovative, evidence-based practices and technologies into their clinical work.
Social Responsibility: As faculty, we instill a strong sense of ethical practice and social responsibility in our students, guiding them to become advocates for occupational justice and health equity.
OTA Program Vision
The vision of the Occupational Therapy Assistant Program is to be a pioneering leader in occupational therapy education, shaping future OTAs with cutting-edge knowledge, clinical expertise, and a commitment to compassionate, client-centered care, rooted in evidence based practice to meet the evolving needs of diverse communities.
Program Outcomes
- Apply ethical standards and safety guidelines during the Occupational Therapy (OT) Process.
- Apply knowledge of global practices, scientific practice, medical terminology and anatomy and physiology in order to demonstrate the basic tenets of entry-level occupational therapy practice.
- Assist in evaluation and screening processes by gathering data, administering assessments, assisting with interpretation, reporting results and collaborating with Occupational Therapists to establish goals.
- Perform interventions by planning, selecting, implementing, grading according to activity analysis, modifying intervention plans and therapeutic use of self.
- Communicate in all formats, written, oral, nonverbal and electronic, with a diverse client population, interdisciplinary team members and the public in a professional and effective manner.
- Display professional behaviors through self-responsibility, response to feedback, work behaviors, time management, interpersonal skills and cultural competence.
- Prepare to sit for the National Board for Certification in Occupational Therapy (NBCOT) exam.
Professional Requirements and Technical Skills
Occupational Therapy Assistant Program, Essential Functions
- These technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the program at Baker College. The College complies with the requirements and spirit of Section 504 of the Rehabilitation Act and the Americans with Disabilities Act of 1990. Therefore, the College will endeavor to make reasonable accommodations for participants with disabilities who are otherwise qualified.
- Effectively communicate in English, both verbally and in writing, utilizing accurate and appropriate terminology with classmates, faculty, clients, caregivers, families, members of the healthcare team and with individuals of all ages, races, genders, socioeconomic and cultural backgrounds.
- Access information from books, reference manuals, computers and paper and electronic medical records to accurately perform job functions and duties.
- Observe clients’ response before, during and after treatment in close and distant proximity to maintain client safety and assess their performance
- Perform or assist with and/or transfer, lift, move, position and manipulate the client.
- Transport heavy, wheeled equipment and clients in wheelchairs and/or stretchers.
- Demonstrate motor skills for safe and effective client-centered intervention.
- Provide assessment and treatment for clients with varied disabilities including clients who may be terminally ill, have transmittable diseases, psychiatric disorders, developmental disorders and other conditions.
- Utilize technology for coursework and client-centered interventions. Perform continuous physical work to fulfill clinical education course requirements.
- Demonstrate appropriate professional and procedural judgment decisions under stressful and/or emergency conditions, emergent demands and a distracting environment.
- Recognize potentially hazardous materials, equipment and situations and proceed safely in order to minimize risk of injury to patients, self and nearby individuals by referencing, utilizing and adhering to OSHA requirements such as MSDS (Material Safety Data Sheets) and universal precautions.
- Demonstrate critical thinking skills necessary to assess and reassess the client’s occupational performance including adaptations and analysis of tasks based on best practices.
- Prioritize, organize and utilize time-management skills to fulfill clinical and course requirements.
- Adhere to HIPAA, American Occupational Therapy Association (AOTA) professional standards and Code of Ethics established by the American Occupational Therapy Association, Baker College professional conduct guidelines and clinical site policies and procedures.
Licensure Requirements
Graduates of an accredited OTA program are eligible to sit for the national certification examination for the occupational therapy assistant, administered by the National Board for Certification in Occupational Therapy (NBCOT). After successful completion of this exam, the individual will be a Certified Occupational Therapy Assistant (COTA) and may apply for licensure in the state of Michigan (and/or any other state in which the person may wish to practice). Please note that national certification and state licensure are mandatory in order to practice in Michigan.
Curriculum Design - Sequencing of Courses
Fieldwork/Clinical Requirements
Each student must complete four fieldwork experiences. Two level I experiences and two Level II experiences.
-
Level I Fieldwork: The design for the Level I fieldwork experience allows for the integration of academic course work with direct application of occupational therapy principles and techniques pertaining to the clinical setting. The intended emphasis of a Level I fieldwork experience is to provide the basic acquisition of observation, professionalism and learning skills in the clinical settings. Level I Fieldwork A takes place in the fall semester and consists of 40 hours experience in a mental/psychosocial or emerging practice area. The Level I Fieldwork B experience occurs in the spring semester and consists of 40 hours in a physical dysfunction setting. Level I experiences are in addition to in class sessions. Level I hours are completed weekly over the course of the semester.
-
Level II Fieldwork: Each student must complete two (Level II Fieldwork A and Level II Fieldwork B), full-time eight-week, Level II fieldwork experiences. For Level II credit, students will need to complete the required weekly full-time hours and the required number of weeks. Placement in level II fieldwork experience begins in the fall semester following the completion of academic course work. All Level II experiences must be completed within 16 months following completion of academic course work.
-
Travel: Due to the availability of quality placements, students may be required to travel up to 90 minutes each way for Level I and 70 minutes each way for Level II.
-
Out of state and International Placements: The program does not utilize out of state or international fieldwork placements (Level I or Level II).
Lab Participation
Students will participate in lab sessions in which they will play the role of the “occupational therapy assistant” in order to learn skills that will be required in the clinical setting. Additionally, students will participate in lab sessions in which they play the role of a “patient” in order to enhance fellow classmates’ learning experiences. Maintaining individual privacy and modesty, as practiced in the clinical setting, is expected of all lab participants, regardless of the role the individual assumes. Should a student be asked to participate in any scenario for which they have a medical condition that is contraindicated, they are responsible for immediately and confidentially notifying the course instructor.
MASTER OF SCIENCE, OCCUPATIONAL THERAPY
Program Overview
The delivery of the Occupational Therapy program at the graduate level revolves around instructors facilitating learning through problem-based case management. Students in the MSOT program will be required to utilize theory, logic, clinical reasoning and pragmatic skills in an interactive learning environment. It is expected that students will participate in discussions and debates and develop treatment choices based on sound research and theoretical assumptions. The Master of Occupational Therapy curriculum emphasizes mastery of the skills required for entry-level practice. The curriculum is designed so that graduates can review, understand, conduct and interpret research activities. Evidence-based practice initiatives make it essential that practitioners’ research skills are well developed.
A felony conviction may affect a graduate’s ability to sit for the NBCOT examination or attain state licensure.
Accreditation Information
The Occupational Therapy Program is fully accredited by:
Accreditation Council for Occupational Therapy Education (ACOTE)
7501 Wisconsin Avenue, Suite 510E, Bethesda, MD 20814
Phone: (301) 652-6611; Website: https://acoteonline.org/
Graduates are eligible to take the national certification examination.
State and National Organizations
- The American Occupational Therapy Association (AOTA)
- The Michigan Occupational Therapy Association (MiOTA)
Mission
The mission of the Occupational Therapy Program is to provide each student with quality graduate educational experiences grounded in the theoretical constructs of occupational therapy. Advanced academic achievement and scholarship are central to developing lifelong learners committed to service.
Program Philosophy
The Baker College Occupational Therapy program defines “occupations as activities that bring meaning to the daily lives of individuals, families and communities and enable them to participate in society” (AOTA, 2017). The program seeks to prepare students who will “promote the health and wellness, remediation or restoration, health maintenance, disease and injury prevention and compensation/adaptation “(AOTA, 2017) of people organizations and populations through engagement across the lifespan.
Our philosophy reflects that of the American Occupational Therapy Association (2017) in that individuals are complex and diverse beings engaged in a dynamic process of interaction with the physical, social, temporal, cultural, psychological, spiritual and virtual contexts. The faculty believe that experiential learning is the ideal method to instill the core concepts of client centeredness, occupational engagement, professional ethics and clinical competence in future generations of occupational therapists.
Program Outcomes
- Apply knowledge of global practices, scientific practices, medical terminology and anatomy and physiology in order to demonstrate the basic tenets of entry-level occupational therapy practice.
- Utilize critical thinking skills to administer assessments in a uniform manner; to ensure findings are valid and reliable.
- Adjust assessment procedures based on the client’s needs, behaviors and culture.
- Establish accurate and appropriate treatment plans based on the evaluation results, through integrating multiple factors such as client’s priorities, context(s), theories, and evidence-based practice.
- Implement intervention plans that are client-centered.
- Satisfactorily produce the volume of work (treatment, documentation and administrative duties) required in the expected timeframe.
- Clearly and effectively communicate verbally, nonverbally and electronically with clients, families, significant others, colleagues, service providers and the public
- Demonstrate consistent work behaviors including initiative, preparedness, dependability and work site maintenance.
- Demonstrate problem solving and critical thinking skills by adhering to ethics of the profession, safety regulations and judgment in safety in regards to self and others throughout the occupational therapy process.
- Prepare to sit for the National Board for Certification in Occupational Therapy (NBCOT) Examination.
- Demonstrate an appreciation for the complexity of context and diversity (including but not limited to socio-economics, culture, gender, race/ethnicity, religion, disabling conditions and sexual orientation) on engagement in occupation.
Licensure Requirements
Graduates of an accredited Masters of Occupational Therapy program are eligible to sit for the national certification examination for the occupational therapist administered by the National Board for Certification in Occupational Therapy (NBCOT). After successful completion of this exam, the individual will be a Certified Occupational Therapist and may apply for licensure in the state of Michigan (and/or any other state in which the person may wish to practice). Please note that national certification and state licensure are mandatory in order to practice in Michigan.
Professional Requirements and Technical Skills
Essential Functions and Technical Requirements The essential functions required by the curriculum are in the following areas: motor, sensory, communication and intellectual (conceptual, integrative, quantitative abilities for problem solving and the behavioral and social aspects that impact the performance).* Technical requirements as distinguished from academic standards, refer to those physical, cognitive and behavioral abilities required for satisfactory completion of all aspects of the curriculum and the development of professional attributes required of all students at completion of their program. These essential functions and technical requirements are referred to as the “Essential Functions.”
These Essential Functions are not conditions of admission to the College or the program. The Essential Functions provide information regarding continued eligibility in this program. A student may be qualified for and admitted to the program, but later be redirected due to a failure to develop and exhibit the Essential Functions. Persons interested in applying for admission to the program should review this information to develop a better understanding of the physical abilities and behavioral characteristics necessary to successfully complete the program.
- Cognitive abilities necessary to master relevant content in courses at a level appropriate by the College. These skills may be described as the ability to comprehend, memorize, analyze and synthesize material in a timely manner. The student must maintain the minimum grade point average (GPA) determined by each program in order to continue with coursework to complete a chosen degree. Students must have a cumulative GPA of at least 3.0 to graduate from any program; however, please note that some programs require a higher GPA in order to continue with coursework.
- Ability to assess all information. The student must be capable of responsive and empathetic listening to establish rapport in a way that promotes openness on issues of concern and sensitivity to potential cultural differences.
- Emotional stability to function effectively under stress and to adapt to an environment, that may change rapidly without warning and/or in unpredictable ways.
- Ability to master information presented in coursework in the form of lectures, written material and projected images and the ability to seek and synthesize information from appropriate and varied sources.
- Ability to recognize one’s own limits, both personally and professionally, as related to one’s skill and knowledge.
- Ability to effectively communicate in English, both verbally and in writing, using accurate and appropriate terminology with classmates, faculty and individuals of all ages, races, genders, socioeconomic and cultural backgrounds.
- Ability to use computers and related technology.
- Ability to prioritize, organize and utilize time management skills.
- Ability to identify, recognize, maintain and disseminate accurate information.
- Ability to correctly interpret and/or clarify, verbal and written communications.
- Ability to conduct oneself in a professional manner including use of appropriate verbal and nonverbal responses in social interactions. Interactions may include physical contact with all people regardless of age, race, gender, socioeconomic and cultural backgrounds
- Ability to think critically and demonstrate problem-solving skills.
- Ability to perform all essential functions related to my program of study in a safe and effective manner minimizing risk to self, patient and others.
- Ability to fulfill requirements of productivity and varying workloads.
- Ability to demonstrate appropriate professional and procedural judgment decisions.
- Ability to adhere to professional standards and Baker College professional conduct guidelines, policies and procedures. These include but are not limited to: Disclosure of any new felony charges, after the initial enrollment process at Baker College, to program officials.
Students are required to disclose any criminal charges that occur while in the program. Failure to disclose any felony charge to the program officials may result in immediate dismissal from the MSOT program.
Participation
Active participation is encouraged in all courses. Students will frequently be involved in discussions, work in groups, and collaborate on in-class learning assignments. It is essential for each student to participate fully and equally when given group assignments. Also, important, is the ability and willingness to provide critical feedback to peers. Many class assignments will include group work and peer reviews.
Project planning, time management,and contingency planning are essential in all professional activities, not just academic coursework. Unless otherwise noted, assignments are typically due at 11:59pm eastern standard time. Faculty can make late work exceptions at their discretion for situations that are isolated, temporary, and resolvable. Faculty should accommodate significant extenuating circumstances outside of the student’s control. The instructor may request supporting documentation. Furthermore, as a general practice, extra credit work is not permitted or the resubmission of already-graded work for a better grade.
It is the responsibility of the student to notify the instructor if absent and arrange with classmates for missing content. Experiential learning is the foundation of the program and involves a combination of lecture and discussion, followed by application (occupational performance). Several classes will involve field trips, guest lectures, observations, and clinical experiences.
Requirements for Graduation
The graduate program consists of four semesters on campus and six months off campus completing Level II Fieldwork. Upon completion of all academic coursework, students are eligible for Level II fieldwork placements (OCC 6750 and OCC 6850). A student must be in good academic standing (graduate GPA of 3.0 or better) to proceed to Level II fieldwork. The fieldwork requirements must be fulfilled within 12 months of completing all academic courses.
The Occupational Therapy program follows the standard graduate school grading scale. The grade and academic appeal process is consistent throughout the Baker College System. Details are outlined in the Baker College Student Handbook. If a course grade is below a 72% (C) the student will be dismissed from the program. Re-application is allowed one time at the graduate level. Re-application will be reviewed by the dean/program director and faculty. Re- admission is not a guarantee.
The maximum number of discontinued or unsuccessful Level II fieldworks (whether Withdrawn, Failed, Incomplete, or Non-credit) is one. If a student fails a fieldwork experience, he/she must successfully pass a repeated fieldwork experience. Only one repeat of Level II Fieldwork will be allowed (OCC 6750 or OCC 6850).
A cumulative GPA of 3.0 is required for graduation.
Curriculum Design - Sequencing of Courses
Leave of Absence
Any student who requests a leave of absence (LOA) from the program must meet with the Program Director/Dean and submit a written request. The request must indicate the student’s plan for return including resolution of any original issues resulting in the LOA. A leave of absence will only be granted for one year thus allowing the student to join the next graduating class. However, students will not automatically be granted re-admittance. Academic standing and resolution of original issues will be considered. Refer to Clinical Fieldwork requirements for LOA or deferment of Level II clinical placements.
Clinical Fieldwork
There are three Level I fieldwork courses at the graduate level. The first is focused on adults with physical dysfunction, the second on children with cognitive and/or physical dysfunction, and the third with psychological and/or social focus. Details of these courses will be explained by the instructors. These requirements involve out of class attendance at a clinical site.
Upon completion of all academic coursework, students are eligible for Level II fieldwork placements (OCC 6750 and OCC 6850). Each student will be assigned two - 12-week clinical affiliations to be completed in the spring and a portion of the summer semester of the final year of the program. It is the responsibility of the Fieldwork Coordinator to assign students to specific clinical sites.
A student must be in good academic standing (graduate GPA of 3.0 or better) to proceed to Level II fieldwork. The fieldwork requirements must be fulfilled within 12 months of completing all academic courses.
The academic fieldwork coordinator, with input from the faculty, will place each student. Students are not to contact facilities concerning clinical placements.
Travel: Due to the availability of quality placements, students may be required to travel up to 90 minutes each way for Level I and 70 minutes each way for Level II. Out of state placements are available upon request, but not guaranteed. The program does not utilize international fieldwork placements (Level I or Level II).
Level II fieldwork is a full-time commitment without pay. Students will work the
same full-time schedule as their OT clinical supervisor. Nontraditional schedules, such as four (4) days at ten hours each are becoming more common, as are weekend and holiday hours. Students are strongly encouraged to begin planning now for this financial and time commitment.
Much preplanning and coordination of information is required in order to secure meaningful experiences on the student’s behalf. There will be several fieldwork preparation meetings, at times scheduled in addition to class time. Students will complete a variety of preparatory activities, certifications, and health checks and to maintain a Fieldwork Portfolio notebook containing documentation of these activities. It is also possible that additional screens and background checks will be required by the clinical site. The cost of these requirements is the student’s responsibility. Students should confirm the dress code with the clinical site prior to the first day of the placement. Some fieldwork sites will provide a name tag but if not, your Baker College Clinical ID will be appropriate.
PHYSICAL THERAPY ASSISTANT
Program Overview
The Physical Therapist Assistant (PTA) is a technical healthcare worker who performs patient care under the supervision of a licensed physical therapist. Typical settings include hospitals, rehabilitation clinics, private practice, geriatric care facilities, sport medicine centers, school systems and industrial sites. For information about the licensure examination see www.fsbpt.org/ExamCandidates.
Accreditation Overview
The Baker College Physical Therapist Assistant Program is accredited by:
Commission on Accreditation in Physical Therapy Education (CAPTE)
3030 Potomac Ave, Ste 100, Alexandria, VA 22314
Phone: 703-706-3245
Web address: www.capteonline.org
E-mail: accreditation@apta.org
Graduation from a physical therapist assistant education program accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE), 3030 Potomac Ave, Ste 100, Alexandria, VA 22134; phone; 703-706-3245; accreditation@apta.org is necessary for eligibility to sit for the Physical Therapist Assistant licensure examination, that is required in all states.
It is the Program Director’s responsibility to ensure that all accreditation activities and requirements are met and that the PTA Program remains compliant with CAPTE accreditation standards and policies. Specifically, the Program Director is responsible for:
- Submission of the required fees and documentation, including reports of graduation rates, performance on state licensing or certification examinations and employment rates
- Notification of expected or unexpected substantive change(s) within the program and of any change in institutional accreditation status or legal authority to provide postsecondary education
- Coming into compliance with accreditation criteria within two years or the length of the program, whichever is shorter
State and National Organizations (Membership)
The American Physical Therapy Association (APTA) is a professional organization that represents Physical Therapists, Physical Therapist Assistants and Students of Physical Therapy. Members are represented by national leadership, chapters and special interest sections.
The Vision Statement for the Physical Therapy Profession, adopted by the APTA in 2013, is as follows: Transforming society by optimizing movement to improve the human experience. Membership is required during the PTA Program. APTA members will have online access to valuable resources including clinical practice guidelines and current evidence. Members will also receive a discount on conferences and continuing education courses. Being an APTA member at graduation allows the student to receive a significant discount on membership up to 4 years post-graduation if renewed within 6 months after the expiration of the student membership.
American Physical Therapy Association (APTA)
1111 N Fairfax St, Alexandria, VA 22314 800-999-2782
www.apta.org
APTA Special Interest Sections: http://www.apta.org/Sections/
APTA Michigan Chapter
Michigan Physical Therapy Association (MPTA)
www.mpta.com
Goals
The goal of this program is to provide students with appropriate didactic and clinical experience leading to successful licensure and entry-level employment in the profession of physical therapy.
Mission
Our mission for the Physical Therapist Assistant Program is to graduate students who have obtained the knowledge and skills to become employed as licensed physical therapist assistants and become contributing members of the physical therapy profession and health care team in diverse settings.
Philosophy
The faculty and administrators of the Physical Therapist Assistant Program believe that technical, interpersonal and critical thinking skills are important components of a quality educational experience. In addition, teamwork, ethics and problem-solving skills are emphasized throughout the educational experience to ensure graduation of competent physical therapist assistants.
Program Outcomes
- Exhibit professional and ethical conduct that reflects expectations of society and other members of the profession, APTA Standards of Ethical Conduct, and APTA Values-Based Behaviors for the Physical Therapist Assistant.
- Using knowledge of scientific practice, anatomy and physiology and disease processes, performs in a safe manner that minimizes the risk to patient, self and others.
- Use inter-professional teamwork to facilitate effective patient outcomes.
- Demonstrate sensitivity to individual and cultural differences in all aspects of physical therapy services.
- Communicate verbally and non-verbally with the patient, caregivers and other healthcare team members in an appropriate and effective manner.
- Demonstrate critical thinking skills related to life span and across the continuum of care, as part of assessing patient status in order to implement and/or modify interventions, performed under the supervision of the physical therapist.
- Performs safe and competent treatment interventions across the lifespan, consistent with the plan of care established by the supervising physical therapist.
- Complete thorough and accurate documentation and billing in a timely manner consistent with legal and ethical standards.
- Perform self-assessment to identify individual learning needs and implement plans for lifelong learning and career development, including, participating in public activities that promote health and wellness.
- Prepare to sit for the National Physical Therapist Assistant Exam (NPTAE).
Code of Ethics
APTA Standards of Ethical Conduct for the PTA
Students are required to abide by the APTA Standards of Ethical Conduct for the PTA at all times inside and outside of the classroom and during clinical education experiences. This includes remaining professional during personal contact with other students and patients, verbal and nonverbal communication and protection of confidentiality and privacy. Students are not allowed to practice physical therapy outside the supervised lab or clinical experiences. Students who fail to comply with this policy will assume full risk and responsibility for their actions and the malpractice insurance provided by Baker will not apply. Students will not attempt to give or receive medical advice within or outside the Program.
Use of the title PTA
The practice of physical therapy is legally regulated in Michigan by the Public Health Code. Section 333.18720 states “An individual shall not engage in the practice of physical therapy or practice as a physical therapist assistant unless licensed or otherwise authorized under this part.” (2020 Legislative Council, State of Michigan). If planning to practice outside of Michigan, students should refer to the practice act defined by the state for information.
Safety Requirements
The following health requirements have been developed to maximize both student and patient health and safety:
- Any significant change in a student’s health status requires written notification to the Program Director. This includes any addition of medication or health conditions with the potential to cause impairment in movement, judgment, vision, thought processes and ability to perform safely in the lab or clinic. Each case will be considered on an individual basis and could require consultation with a physician or the submission of medical records.
- Students who become pregnant during the program are encouraged to complete a pregnancy waiver form at least quarterly that is signed by their physician and includes any limitations. The form is to be completed at each physician visit in the 3rd trimester.
- It is the PTA Program’s responsibility to ensure that all lab equipment and classroom materials are well-maintained and in safe and proper working order. Students are not allowed to use equipment that they have not been instructed on. Safe use of equipment procedures are posted in the lab. Mechanical equipment is inspected and calibrated yearly by Patterson Medical and current inspection stickers are present on all electrical and mechanical equipment in the lab. Non-mechanical equipment is inspected quarterly by the PTA faculty and replaced as needed. If equipment is deemed unsafe for use it will be removed from the lab immediately and the problem will be reported to the Program Director. Students, faculty and staff in the lab are responsible for reporting any equipment concerns or safety issues immediately to the Program Director.
- Students are expected to practice universal precautions in the event of possible exposure to hazardous materials or bodily fluids in the lab or clinic. Students will be instructed on proper precautions in the event of an emergency or exposure during the first lab-based course (PTA 2310) and are expected to use sound judgment and precautions as necessary throughout the program. This includes infection control protocols such as handwashing and wearing personal protective equipment as appropriate.
- Students have the right to be treated with safe and reasonable care by other students when practicing during lab sessions and open labs and during practical examinations. If at any time a student feels that his/her safety is at risk he/she should report it to an instructor and appropriate action will be taken immediately. In the event of an incident of injury or harm occurring during classroom or lab sessions or open labs, students should report immediately to the instructor and seek the proper medical care.
PTA students will have access to the PTA lab during non-class hours provided the following conditions are observed to ensure safety:
- A lab assistant or instructor is on campus.
- Friends and Family are not allowed in the lab.
- All students must be able to locate the emergency call box. This item will be identified on the first day of orientation.
- All students must be able to identify emergency evacuation procedures located by the door of the lab.
- Students are only allowed to practice techniques that have been previously discussed in class, no other procedures are allowed.
- In case of an emergency, please contact Campus Safety.
- Campus Safety: All students must have their student badges on them at all times while on campus. In the event of an emergency, call the Campus Safety office. Please notify the dispatcher that a student is reporting an emergency or a crime and provide them with the location and related information. Members of the campus safety department are police empowered with all rights and responsibilities of their position. The Campus Safety Office also provides escort service and students can call the office to request an escort on campus or to their vehicle if they feel unsafe at any time.
- Off-campus safety: The same safety policies and procedures apply to students involved in off-campus activities such as field trips, off-campus laboratories and off-campus clinical experiences. In addition, students are required to follow the safety policies and procedures of the specific clinical education site at which they are a student. A field trip form is to be completed by the course instructor and field trip site prior to the field trip which outlines student safety and site responsibilities.
Professional Requirements
The PTA Program at Baker College abides by the professional standards set forth by the APTA and behavioral expectation of the Generic Abilities document.
Core Values
Students are expected to demonstrate the seven core values of the profession of physical therapy as defined by the APTA Core Values Document. Students will refer to and apply the Core Values throughout the technical program and be expected to demonstrate professionalism in all aspects of the student experience.
Values-Based Beaviors of the PTA
Students are required to behave in a manner consistent with the Values-Based Behaviors of the PTA established by the APTA. Students will be required to periodically assess their behaviors according to these standards and reflect on ways to alter behaviors accordingly.
Professional Behaviors for the 21st Century
Throughout the curriculum the PTA Program assesses student behaviors based on the Professional Behaviors for the 21st Century (2009-2010) which consist of 10 categories of behavioral expectations that have been determined to be essential to the successful performance of the duties of a PTA or PT.
Student Professional Development Portfolio
Professional Development as a Physical Therapist Assistant encompasses commitment to learning, commitment to service and commitment to the profession of Physical Therapy. To promote development, each student will create a portfolio including experiences in these areas over the next year.
Professional Development Portfolio Requirements:
-
Service Learning (4 hours required to graduate from the PTA Program)
-
Volunteer activities that benefit non-profit organizations or educational institutions
-
Activities must be related to the field of Physical Therapy
Academic Requirements
Reapplication after Academic Dismissal
Students dismissed from the PTA Program for academic reasons may reapply to the program one more time with the approval of the Program Director. Students meeting this criterion may opt to apply to the campus of their choice (OW, RO or MU). Students reapplying to the program must complete the PTA program reapplication process including submitting a new application. Students will be required to demonstrate competency in all PTA technical curriculum prior to withdrawal, which may include: auditing courses, re-taking courses and/or completing practical exams.
Reapplication After Voluntary Withdrawal
Students accepted in the Physical Therapist Assistant Program who choose to voluntarily withdraw due to non-academic reasons will be eligible for reentry into the program one time. Reentry must occur within one year of approval of the program director. Any requests for withdrawal and/or re-entry must be submitted to the Program Director in writing. If it has been more than one year since the student has taken DMS major courses, the Program Director may set specific conditions necessary to bring the student to the proper level of competency prior to re-entry. This may include the need to retake previous courses and/or demonstrate knowledge and competency in regards to their didactic and clinical skills.
Program Dismissal for Behavioral Violations
Students dismissed for behavioral reasons including professional and/or ethical violations will be ineligible for reapplication to the physical therapist assistant program on any Baker College campus.
Technical Skills
In addition to the sensory, psychomotor, cognitive and communication requirements identified in the CoHS Student Handbook, the following technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the PTA Program at Baker College:
- Access information from books, reference manuals, computers and paper and electronic medical records to accurately perform job functions and duties.
- Observe clients’ response before, during and after treatment in close and distant proximity to maintain client safety and assess their performance.
- Physically move, position and transfer patients of varying ages, sizes and abilities.
- Transport heavy, wheeled equipment and clients in wheelchairs and/or stretchers.
- Demonstrate motor skills for safe and effective client-centered intervention.
- Provide assessment and treatment for clients with varied disabilities including clients who may be terminally ill, have transmittable diseases, psychiatric disorders, developmental disorders and other conditions.
- Utilize technology for coursework and client-centered interventions.
- Perform continuous physical work to fulfill clinical education course requirements.
- Demonstrate critical-thinking skills necessary for clinical decision making and problem solving.
- Demonstrate appropriate professional and procedural judgment decisions under stressful and/or emergency conditions, emergent demands and a distracting environment.
- Recognize potentially hazardous materials, equipment and situations and proceed safely in order to minimize risk of injury to patients, self and nearby individuals by referencing, utilizing and adhering to OSHA requirements such as MSDS (Material Safety Data Sheets) and universal precautions.
- Adhere to HIPAA, professional standards and code of ethics established by the American Physical Therapy Association, Baker College conduct guidelines and clinical sites policies and procedures to fulfill requirements of rotating schedules and heavy workloads and demonstrate personal accountability for actions and decision outcomes.
Supervision Requirements
Medicare defines the title of Physical Therapy Assistant as “a person who is licensed as a physical therapy assistant, if applicable, by the state in which practicing and has graduated from a 2-year college level program approved by the American Physical Therapy Association.” (42 CFR 485.703 Personnel Qualifications (c) (5)).
Blue Cross Blue Shield of Michigan defines the Physical Therapist Assistant as “one who has an associate degree from an accredited physical therapist assistant program and meets the state of Michigan’s legal requirements.” (Guide for Providers, Glossary).
Therefore, until a student has completed their AAS degree, they cannot promote themselves or their services as a PTA. This constraint also applies if during a student’s education, they are employed as a physical therapy technician or aide. The skills and techniques taught in this program exceed those of an aide and should not be applied inappropriately in the clinic.
Licensure Requirements
Students must complete the following to be eligible for PTA Licensure in Michigan:
- Graduate from a physical therapist educational program that is accredited by the Commission on Accreditation in Physical Therapy Education (CAPTE).
- Complete and submit application for licensure and fee, along with supporting documents to Michigan State Board of Physical Therapy.
- Complete fingerprint report and criminal background check from an authorized agency.
- Pass Jurisprudence exam
- Pass the National Physical Therapy Examination (NPTE) that is administered through the Federation of State Boards of Physical Therapy (FSBPT).
- Applicants for licensure must schedule, complete and pass the jurisprudence examination through PSI. PSI can be contacted by visiting www.psiexams.com or by calling PSI at 800-733-9267.
Curriculum Design - Sequencing of Courses
Competencies
There are 8 courses in the PTA program that have lab components. These labs each have 4-5 “skill checks” or “competencies” which must be completed and passed successfully before taking the Cumulative Final Lab Practical at the end of each semester. The number of skill checks or competencies varies for each class depending on the material covered. Some competencies may be combined.
Each skill check, competency and final lab practical contains “critical safety” and “critical competency” elements that must be performed consistently throughout the test. Failure to demonstrate any “critical safety” or “critical competency” element results in an automatic failure of the skill check, competency or lab practical.
Students will be responsible for practicing skills during open lab times. Even though lab assistants will be present, the students are responsible for independent learning and practice.
Refer to the PTA Clinical Competency Notebook for further details.
Clinical Hours
The clinical education component of the PTA Program is designed to give students an opportunity to assimilate and apply the concepts learned in the technical coursework. The following courses are required for successful completion of the PTA Program:
PTA2710 Clinical Education I (2 weeks, 80 hours) Beginning of 3rd Semester PTA2720 Clinical Education II (8 weeks, 320 hours) Final Semester
PTA2730 Clinical Education III (8 weeks, 320 hours) Final Semester
More specific information regarding clinical sites and dates will be given to students during the Professional Preparation course (PTA 2510).
Under no circumstances should students contact clinical sites to arrange placements. The Director of Clinical Education (DCE) and other faculty in the PTA Program have put a considerable amount of time into developing collaborative relationships with the clinical faculty, including the arrangement of contractual agreements. All site contacts will be made by DCE. Students are expected to bring any questions or concerns about clinical education to the DCE in a timely manner.
The students’ preferences for site selection will be considered during the assignment of clinical sites, but the final determination will be that of the DCE. Clinical education is an essential learning experience and it is the student’s responsibility to fulfill the obligations set forth by the specific sites regarding hours, performance and supervision. The DCE is responsible for assigning final grades for the Clinical Education Courses.
RADIOLOGIC TECHNOLOGY
Program Overview
Radiologic imaging is often the first step in identifying, diagnosing and treating many diseases and is an increasingly common part of many medical procedures and regimens. Performing diagnostic imaging procedures requires training, skill and experience to fully understand the technical standards of the radiologic sciences and provide quality healthcare. Radiologic technologists perform most of their work independently but only do procedures that are prescribed by a physician or midlevel provider. Final images resulting from the procedures are not interpreted for medical diagnosis by the radiologic technologist, but rather a radiologist, emergency physician or orthopedic surgeon as indicated by each situation.
The radiography curriculum is based on two years of full-time study. Once admitted into the program the student will complete two semesters of full-time course work on campus. The student then completes two semesters of full-time (40-hours a week) clinical rotation. All major core courses must be completed with a 2.7 GPA (B-) or better prior to the start of the program courses and throughout the program and clinical semesters.
The clinical experience segment of the program is a time of application and skill development. It occurs during the last two semesters of study and is completed at a clinical affiliate hospital. The location of the clinical affiliate may require that a student relocate or perhaps have a longer commute to the assigned location.
Students have been given all necessary resources to begin a combination of self-directed and faculty directed review of theory provided during the first year of study. The focus of the clinical year of the program is the learning and expansion of applied knowledge. The student will also discover during this time that a significant portion of practical knowledge can only be gained within experiences of an assigned clinical environment. This time of application and professional growth is not a situation of employment with the clinical site. If the student receives an offer of employment during clinical training, it will be expected that the separation of roles as a student and employee are maintained as part of professional conduct.
Students are required to purchase/obtain radiographic lead markers and scrubs.
Students are required to obtain/maintain CPR certification and provide proof of it to program officials.
Accreditation Information
The Baker College Radiologic Technology program is nationally accredited by:
Joint Review Committee on Education in Radiologic Technology (JRCERT)
20 Wacker Drive, Suite 2850, Chicago, IL 60606-3182
Phone: (312) 704-5300
Fax: (312) 704-5304
State and National Organizations
https://www.msrt.org/
State Representation to the ASRT, Continuing Education and Scholarships
Goals
-
Students will perform competently
-
Students will critically think and solve problems effectively
-
Students will communicate effectively
-
Students will develop and grow professionally
-
Students will become successful graduates of the program
Mission
The mission of the Baker College Radiologic Technology program is to enable qualified students to develop into competent and professional entry-level radiographers who are prepared to successfully sit for the ARRT examination and acquire gainful employment. We believe that this is done through exercises in critical thinking, varied clinical experience, the encouragement of universally responsible behavior and foundations in guiding radiologic principles.
Program Outcomes
By the end of the Radiologic Technology Program, students will be able to:
Competence
Critical Thinking
Communication
-
Demonstrate oral communication skills that exhibit patience and empathy with patients regarding their health history and prescribed radiologic procedures.
-
Use concise oral and written communication with physicians and members of the interdisciplinary team to provide optimal care to patients.
Professionalism
-
Investigate the importance of professional growth, including continuing education, professional societies, career development and participating in activities that promote the radiologic profession.
-
Recognize the diverse needs of patients and co-workers.
-
Demonstrate the knowledge and skills necessary to successfully take the American Registry of Radiologic Technologist’s Examination for Radiographers.
-
Demonstrate professional behaviors and skills consistent with a preferred entry-level radiologic technologist.
Code of Ethics
The Baker College Radiography Program expects all participants to abide by the national code of ethics for the practice of radiologic technology, which is regularly reviewed and revised as necessary by the American Society of Radiologic Technologists when advances to technology and patient care occur. Ethical standards are enforced by the
American Registry of Radiologic Standards and Code of Ethics.Professional Requirements and Technical Skills
These technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the program at Baker College. These standards are not conditions of admission to the program. Persons interested in applying for admission to the program should review this information to develop a better understanding of the physical abilities and behavioral characteristics necessary to successfully complete the program. The College complies with the requirements and spirit of Section 504 of the Rehabilitation Act and the Americans with Disabilities Act of 1990. Therefore, the College will endeavor to make reasonable accommodations for participants with disabilities who are otherwise qualified.
-
Access information from books, reference manuals, computers and paper and electronic medical records to accurately perform functions and duties.
-
Comprehend technical and professional materials (i.e. textbooks, journal articles and procedure manuals) to accurately perform clinical testing and/or use of equipment.
-
Explain procedures and treatment appropriate to the patient’s level of understanding including what will be required while respecting patient confidentiality and privacy.
-
Recognize and respond appropriately to distress sounds from patient, audible/visual alarms/signals on patient-monitoring equipment for patient safety.
-
Respond appropriately to changes in the patients’ status before, during and after procedures.
-
Monitor and respond to patient and accessory medical equipment directly and by intercommunication system during procedure to assess patient response and safety.
-
Obtain optimum quality of radiographic images by clear discrimination of shades of gray.
-
Accurately interpret and validate text, numbers and graphs from print and video monitors used for fluoroscopy and digital imaging.
-
Evaluate, synthesize and communicate diagnostic information to the attending radiologist.
-
Recognize and correct performance deviations in imaging.
-
Perform or assist with transferring, lifting, moving, positioning and manipulating the patient.
-
Transport heavy, wheeled equipment and patients in wheelchairs and/or stretchers.
-
Accurately obtain precise measurements and determine appropriate immobilization and positioning aids needed for performing procedures.
-
Provide safe and effective care including but not limited to administration of oral or rectal contrast medium.
-
Perform and document warm-up procedures and quality assurance checks on imaging and treatment equipment.
-
Recognize potentially hazardous materials, equipment and situations and proceed safely in order to minimize risk of injury to patients, selfand nearby individuals by referencing, utilizing and adhering to OSHA requirements such as MSDS (Material Safety Data Sheets), universal precautions, radiation safety standards and policies and procedures.
-
Demonstrate appropriate professional and procedural judgment decisions under stressful and/or emergency conditions (i.e. allergic reaction or cardiac arrest) and a distracting environment (i.e., high noise levels, crowding, complex visual stimuli).
-
Adhere to HIPAA, American Society of Radiologic Technologists (ASRT) professional standards, Baker College professional conduct guidelines, program requirements and clinical site policies and procedures.
Supervision Requirements
All clinical practicum experiences will be under the supervision of a qualified ARRT registered radiographer, Academic Clinical Coordinator and/or Clinical Instructor. Department assignments may direct the student to rotate in a particular setting or with a particular person, designed to assist the student through their training with guidance, support and leadership. In compliance with our Standards, supervision is defined as follows:
Direct Supervision
-
The qualified registered radiographer reviews the requisition for the examination and/or procedure in relation to the student’s achievement and the curriculum level completed.
-
The qualified registered radiographer evaluates the condition of the patient in relationship to the achievements and performance level of the student.
-
The qualified registered radiographer observes the student perform the radiographic exam.
-
The qualified registered radiographer reviews and critics the radiographs with the student and approves all finished radiographs.
-
After demonstrating competency, interns may perform procedures with indirect supervision.
-
The student must continue to be directly supervised during all surgical and mobile procedures, including mobile fluoroscopy, regardless of the level of competency.
Indirect Supervision
Is supervision provided by a qualified registered radiographer who is immediately available (in an adjacent room and able to hear calls for help from the student) to assist the student regardless of the level of the student’s achievements. The use of a phone or beeper is not considered immediately available! The student will continue to be provided with “one-on-one” direct supervision during all surgical and mobile procedures, including mobile fluoroscopy, regardless of the level of competency.
Repeating of Radiographs
In support of professional responsibilities for provision of quality patient care and radiation protection, unsatisfactory radiographs (repeats) shall be repeated only under the direct supervision of a qualified radiographer, regardless of the intern’s level of competency. This is a JRCERT standard for accredited educational programs of radiography. (Form is located in section XI).
The student shall be supervised at all times by program officials when ionizing radiation is on in the lab.
-
The student shall be supervised by hospital personnel designated as a clinical instructor and shall follow the Direct / Indirect Supervision Guidelines while at the clinical site as set forth by JRCERT.
-
Program officials will maintain contact with students via email, phone and regular site visits.
Licensure Requirements
Michigan does not require licensure but many other states do require it. Nearly all hospitals in the United States require certification from the American Registry of Radiologic Technologists. Most states that require licensure base issuance mainly on ARRT certification.
Curriculum Design - Sequencing of Courses
Competencies
Refer to details about the performance, tally and scoring of competencies in the course syllabi. Students must complete all lab-based competency requirements for each course as preparation for clinical training. Clinical competencies are periodically revised and outlined by ARRT. There are three categories of ARRT competencies;
Patient Care Mandatory Procedures and selections that must be made from the elective list of procedures.
Clinical Hours
Clinical experiences occur as eight-hour shifts, five days per week. These participation hours usually occur during normal business hours, but all students are also expected to participate in alternate shifts that occur in the evening and on weekends. Clinical training does not occur during overnight shifts or on holidays when the college campuses are closed. The program has three sequential clinical courses with their participation hours listed as follows.
-
RAD 2310: 560 hours of clinical participation is required along with weekly contributions to online discussions and review activities.
-
RAD 2320: 320 hours of clinical participation is required along with weekly contributions to online discussions and review activities. There will be professional growth and development opportunities with advanced imaging technologies.
-
RAD 2450A: 320 hours of clinical participation. The course also requires additional hours of didactic review.
Radiation Safety
The following rules have been established for the student’s protection against ionizing radiation during laboratory and clinical procedures. These rules are established for the radiologic technology student and must be strictly adhered to.
-
No student is to be permitted into the radiology laboratory or clinical department for observation or clinical experience without radiation dosimeter badges. It is the student’s responsibility to turn in the badge monthly for interpretation. Film badges must be worn at all times during hospital observation, lab and clinical. If protective aprons are used, the appropriate badge must be placed above the apron so that any radiation reaching any part of the body will be recorded.
-
If an emergency arises in which the student must hold and/or support a patient, protective apron and gloves must be worn. Students should not hold patients during any radiographic procedure when an immobilization method is the appropriate standard of care.
-
During the exposure or procedure, the student will not place themselves in direct line with the central ray, even though they are wearing a lead apron. The student shall stand in an area where the tube is pointing away from the student’s body.
-
Under no circumstances will the student permit themselves or fellow students (or any other human being) to serve as patients for test procedures or experimentation.
-
During fluoroscopic procedures the following procedures will prevail:
-
The student will wear a lead apron at all times or they will remain behind a lead protective screen and not in visible line with either tube or patient.
-
The dosimeter badge will be worn as noted above.
-
Stand as far from the patient and tube as possible, consistent with the conduct of the examination.
-
When observing and/or performing radiographic procedures in surgery, the following will prevail:
-
A lead apron will be worn.
-
Stand as far from the patient and tube as practicable.
-
Stand so that the central ray is pointing away from the student’s body.
-
Observe all regulations which apply to work in surgery, such as preserving sterile fields, wearing surgical garments, etc.
-
When observing and/or performing radiographic portable procedures in room occupied by patients, the following will prevail:
-
A lead apron will be worn.
-
A dosimeter badge will be worn.
-
Stand as far from the patient and tube as practicable.
-
Stand so that the central ray is pointing away from the student’s body.
-
Observe all regulations which apply to work in surgery, such as preserving sterile fields, wearing surgical garments, etc.
In addition, during actual exposure, the student must step outside the room if the student cannot stand at least ten feet from the patient.
Radiation Monitoring
In order to ensure proper precautions against radiation accidents, all students shall be provided with dosimeter badges for radiation control and monitoring, in compliance with existing rules and regulations of the Michigan State Board of Health. All standard radiation safety practices with regard to protection to patients and personnel shall be strictly adhered to. Dose monitoring reports (dosimeter) must be turned in by the student to the college each month. Under law, this report must be available to the student. The student must blacken-out all serial numbers on the report except his/her own before turning it into the College.
Exposure Policy
The dose value is calculated as the average of deep, eye and shallow doses unless one of these categories exceeds 40 mrem in a month. Where the recorded value in a single category exceeds 40 mrem in a month, that value will be the evaluated dose.
|
Dose Range and Affected Individual
|
Lab Instructor
|
Lab Student
|
Clinical Student
|
|
Less Than 4 mrem/month
|
A
|
A
|
A
|
|
5-20 mrem/month
|
C
|
D
|
B
|
|
21-40 mrem/month
|
D
|
D
|
C
|
|
Over 40 mrem/month
|
D
|
D
|
D
|
SITUATION A
This is considered an insignificant exposure and may be incidental to badge handling or transit. No action is necessary.
SITUATION B
The individual has received a normal exposure for the functional environment. The value indicates good radiation safety practices. No action is necessary.
SITUATION C
The individual has received a higher than average exposure. This may be due to a special situation where good radiation safety practices were applied but similar incidents of exposure should be kept to a minimum. The individual should take precautions to prevent this from being the consistently received exposure level. The radiation safety officer will investigate and suggest changes in routine if this level of exposure is recorded during the next two consecutive months. Disciplinary action shall be taken if suggestions are not followed. Discipline may include dismissal from the program upon approval of the campus president.
SITUATION D
The individual has received a higher than average exposure that is of special concern. There shall be no continued activities near energized X-ray generating equipment until the radiation safety officer has investigated the exposure and there is documentation of a reasonable and probable explanation. If it is concluded that exposure was caused by poor radiation safety practices by the individual of whom the badge monitors, then disciplinary action will be taken. Discipline may include dismissal from the program upon approval of the campus president.
Radiation Safety Practices for Patients
Students are instructed in the methods and necessity of patient radiation safety throughout the Radiography program. During the clinical internship, the student radiographer will ensure the patient radiation safety practices are employed.
-
The student will appropriately shield all patients for all exams whenever possible. Shielding should not interfere with the imaging procedure.
-
The student will select proper image receptor size and technical factors for each patient.
-
The student will use appropriate collimation.
-
Students must not hold image receptors during any radiographic procedures.
-
Students should not hold patients during any radiographic procedure when an immobilization method is the appropriate standard of care. If an emergency arises in which the student must hold and/or support the patient, the student must wear a protective lead apron and lead gloves.
-
The student will be either directly or indirectly supervised at all times during radiographic procedures.
-
All repeated images will be done under the direct supervision of a registered radiographer. A Repeat Study Notification form will be filled out and submitted for each repeated study indicating the number of images repeated. This form will be forwarded to the Clinical Coordinator.
Baker College MRI Safety Policy
The area in and around the magnetic resonance imaging scanner has unique dangers. Death or serious injury can occur to anyone in the scanning room when common types of metal are brought into the MRI environment. Please note all of the following:
-
In MRI, the magnetic field is always present. Ferromagnetic objects will either become projectiles due to the influence of extreme forces or conduct potentially dangerous amounts of heat due to the microwave energy emitted from the scanner.
-
Allowing any ferromagnetic materials into the scanning area is strictly prohibited in all situations. This includes times when life saving measures are needed. Patients must always be removed from the scan room when the use of restricted equipment is needed (AEDs).
-
Patient care Items such as gurneys, oxygen tanks, IV poles, wheelchairs and immobilization devices must be designed for and approved for use by the MRI department before they can be brought in proximity to or inside of the scanning control / technologist work area or the scanning room.
-
Personal items such as stethoscopes, pens, scissors, phones and credit cards must also be kept away from the scanner and left in an area designated by the MRI staff before you get near to the scanning room.
-
Other hazards include items in or on your body, including iron-containing tattoo dyes, metallic foreign bodies or surgically implanted devices in your body. All students must comply with policies and procedures established at the clinical setting pertaining to the prevention of metallic objects coming in proximity to the MRI suite and most importantly, the MRI scanning room.
In addition to following MRI safety protocols at the clinical setting, you must complete the College’s MRI safety screening form and present it to both your clinical coordinator at the college and MRI technologist staff at the clinical facility. You must have approvals from both based on the information you provide on the form before seeking access to MRI zones III or IV. You must inform your clinical instructor, clinical coordinator and program director in writing if there is a change in your status in regards to your responses on the MRI safety screening form. Baker College MRI Safety Screening Form Coming Soon!
Advisement Regarding Pregnancy
The National Council on Radiation Protection and Measurements recommends that the dose limit equivalent to the embryo-fetus from occupational exposure to the expectant mother should be limited to 0.5 REM for the entire gestational period. Through proper instruction of all safety precautions, personnel monitoring and strict adherence to these precautions, it is possible to limit all occupational exposure to under 0.5 REM per year and prevent fetal dose limit levels from being surpassed.
A valuable part of learning is maintaining a rotation schedule through the various assigned areas without interruption. The student should carefully consider this if she is trying to become pregnant. In any event, the program will assist the student during pregnancy within the provisions of the pregnancy policy.
Should any student suspect pregnancy, they are encouraged to choose to report it immediately to the program director. This is voluntary on the part of the student.
However, failure on the part of a student to notify the Program Director (in writing) of an existing pregnancy shall absolve both the college and the clinical education center (hospital) of any responsibility from an assignment to a radiation area.
Radiation Safety During Student Pregnancy
Student in Lab
-
Offer student a declaration form (“Notice of Pregnancy”) Notice of Pregnancy Form Coming Soon!
-
Have student read NRC Regulatory Guide 8.13
-
Student discusses concerns with the Program Director and decides whether to sign the declaration. Declaration of pregnancy is completely voluntary.
-
Send a Radiation Safety Plan and Program Exposure Policy with the student to her physician. Initial additional restrictions of the program are listed as “none”.
-
Physician and student discuss if or what restrictions to add to the safety plan.
-
Student is double monitored and continues with normal lab activities unless otherwise indicated by a written recommendation submitted by the student and her physician.
-
Students may declare the end of pregnancy status in writing at any time.
Student in Clinical Assignments
-
Student is offered a declaration form (“Notice of Pregnancy”)
-
Student reads NRC Regulatory Guide 8.13.
Regulatory Guide 8.13 can be retrieved from the link or found at the back of this handbook.
-
Student discusses concerns with the program director and decides whether to sign the declaration. Declaration of pregnancy is completely voluntary.
-
The declared pregnant student will be given the opportunity to select from one of the following options for completing the program:
-
Withdraw from the program during the period of the pregnancy and re-enter with the next available offering of the non-completed courses. Within two weeks after the end of pregnancy the student must provide the program director with written notice of intent to re-enter. This provision cannot be used repeatedly.
-
Continue in the program without modification.
-
Continue in the program but adhere to the following:
-
Protection measures, as in ordering a fetal dosimeter for the student cannot be completed until the student has declared pregnancy.
-
The student is advised to limit no more than half of the scheduled clinical experience day participating in portable or fluoroscopy assignments during first and second trimesters.
-
The student is advised to exit the procedure room when a fluoroscopy procedure has exceeded 5 minutes of exposure time (finding a replacement technologist for the procedure if necessary).
-
The student is advised to wear a lead apron that wraps around the entire abdomen when involved in fluoroscopic procedures.
-
Student and physician discuss if or what recommendations to follow.
-
Physicians may offer additional recommendations to the student.
-
Student presents the program director and clinical coordinator with a list of the recommendations that are agreed upon to accept and follow.
-
Consistent with accepted medical practice and pharmaceutical labeling, the student shall avoid all procedures involving the use of methotrexate and/or other chemotherapy agents of which contact is known to present extreme risk to a fetus.
-
Student discusses the plan with the clinical preceptor to assure assistance with following the accepted recommendations.
-
Student is double monitored and continues with a normal clinical activity schedule until delivery. Reasonable accommodations are made to accomplish normal cohort graduation date. Students may declare the end of pregnancy status in writing at any time.
Pregnancy Un-Declaration
The student may at any time, after declaring pregnancy, submit a written notice to the Program Director stating that the student is no longer pregnant. After submitting this written withdrawal of declaration, any restrictions in connection with the pregnancy are void.
Complaints of Program Violation of Accreditation Standards
This following policy only applies to violations of JRCERT Standards. JRCERT will not attempt to resolve issues with individual students. For example, a student may be able to resolve a grading issue by utilizing Baker College’s “academic appeals process”.
Step 1: The student must first discuss the concern in dispute with their instructor. The only concerns that are applicable are non-compliance issues regarding the JRCERT Standards.
Step 2: If the concern is not resolved in Step 1 and the student wishes to pursue the issue, the student must communicate it in writing to the Program Director. Step 2 must take place within 90 days of the incident/observation of non-compliance. The Program Director will give the student an “Allegation of Non-compliance” form which the student will complete and return to the Program Director within seven business days. Upon receipt of the form, the Program Director will immediately investigate the allegation.
Step 3: The Program Director will read the allegation form and investigate the issue of alleged non-compliance. The Program Director will complete a written response to the student’s concern within 7 days of receipt of the notification in writing from the student.
Step 4: If the concern is still not resolved and the student wishes to pursue the allegations, the Program Director will provide copies of any and all documents to the student within 5 business days. The student then must contact the JRCERT directly to obtain the necessary forms and procedures:
Customer Satisfaction Policy
Baker College is an institution focused on student satisfaction. To that end, any concerns or complaints regarding the radiologic technology program (including classroom cleanliness, facilities concerns, and program policies) can be sent to the attention of the director of the program on the appropriate campus. The director will investigate the complaint, consult with all parties involved and provide a response as soon as all information has been evaluated. The program director will inform the dean of the College of Health Science of the complaint, and an investigation will be conducted with appropriate actions to ensure a resolution.
If resolution cannot be reached at the level of the program director, the problem will follow the chain of command, beginning with the dean of the College of Health Science, followed by the chief academic officer/vice president of academics of the campus, the president of the campus and finally the president of the Baker College system.
More information on Concerns and Complaints can be found at the Baker Rad tech website or the Baker RAD Handbook. To file a complaint, please click on the
Concerns and Complaints Link.SURGICAL TECHNOLOGY
Program Overview
The surgical technologist is a skilled person, qualified by didactic and clinical training to provide services in the operating room under the supervision and responsibility of the operating room supervisor and surgeon. Surgical technologists function in association with nurses, physicians, and other health care providers to help provide the best possible care of the surgical patient.
Accreditation Information
The Surgical Technology program is accredited by:
Commission on Accreditation of Allied Health Education Programs (CAAHEP) 9355 -
113th St. N, #7709, Seminole, FL 33775
Phone:727-210-2350 F:727-210-2354
Upon the recommendation of the:
Accreditation Review Council on Education in Surgical Technology and Surgical Assisting (ARC/STSA).
19751 East Mainstreet, Suite #339, Parker, CO 80138
Phone: 303-694-9262
State and National Organizations (Membership)
Mission
The mission of the Baker College Surgical Technology program is to provide a comprehensive education that combines theoretical understanding with practical experience, equipping students with the expertise to assist surgeons in delivering safe, efficient and compassionate surgical care.
Program Goal
The goal of the surgical technology program is to prepare entry-level Surgical Technologists who are competent in the cognitive (knowledge), psychomotor (skills), and affective (behavior) learning domains to enter the profession. The surgical technology program provides a comprehensive education integrating rigorous academic instruction and practical clinical experience. By fostering a deep understanding of surgical procedures, honing technical skills, and cultivating professional attitudes, the program ensures that graduates are well-equipped to deliver high-quality patient care and effectively collaborate as essential healthcare team members.
Program Outcomes
Cognitive
-
Analyze the sequence and rationale behind surgical procedures.
-
Evaluate sterilization and aseptic techniques and their effectiveness in preventing infection.
-
Relate surgical anatomy and procedure to preparation for the surgical case.
-
Apply surgical technology principles to solve problems related to surgical procedures and patient care.
-
Demonstrate comprehensive knowledge and proficient application of surgical pharmacology and anesthesia practices.
-
Explain the perioperative department’s unique environment and operations, including its structure, roles, and protocols.
Psychomotor
-
Assemble, handle, troubleshoot, and pass surgical instrumentation and equipment during surgical procedures.
-
Create, monitor, and maintain a sterile field.
-
Organize instrumentation, supplies, and materials to ensure no retained surgical items.
-
Apply knowledge to correctly handle and label medications and surgical specimens.
-
Identify and appropriately respond to surgical emergencies by performing necessary interventions or assisting the surgical team.
Affective
-
Practice appropriate communication behaviors (verbal and nonverbal) in the clinical setting.
-
Exhibit effective collaboration and teamwork in the surgical environment.
-
Apply feedback, engage in self-reflection, and create a plan for continuing education to demonstrate a continuous learning attitude in surgical technology.
-
Practice culturally appropriate, patient-centered care during all phases of surgical intervention.
-
Exhibit a surgical conscience by adhering to professional, ethical standards and guidelines.
Additional Fees
The following fees are specifically associated with the Surgical Technology Program
Safety Requirements
Students may often be involved with activities and instruction that have the best outcome when hands on instruction is utilized. Certain activities are required elements for the student to successfully complete the program. These lab activities do require that the students participate by working with other students and instructors to learn the skills before being placed into a live patient setting. Activities such as the following may require students to be involved in situations that involve hands on instruction by other students and/or Instructors:
The surgical technology lab is run like an Operating Room and therefore students will be held to the same standards. During lab class time students will be exposed to the following conditions:
-
Prolonged standing or sitting in one place
-
Prolonged retraction of tissues that may be uncomfortable
-
Exposure to sharp objects such as scalpel blades, hypodermic needles, suture needles and cautery tips
-
Poor lighting conditions
-
Pushing or pulling objects or items in excess of 25 pounds
-
Bending, stooping or stretching
-
Chemicals in surgical scrub solutions such as iodine, chlorhexidine, and alcohol
-
Items that may cause irritation to mucous membranes
-
Radiation
The Baker College Surgical Technology program instructs students to follow the Association of Operating Room Nurses (AORN) and, Centers for Medicaid and Medicare infection control policies and thereby enforces the following standards in the laboratory and clinical settings:
-
No false eyelashes/eyelash extensions
-
Nails will be kept short, and clean. No acrylic nails, or nail polish
-
Hair will be kept natural and of a length that is able to be completely contained under a bouffant scrub cap
-
Beards and facial hair will be trimmed and able to be contained beneath a beard cover
-
Make up will be light and natural looking.
-
Facial piercings must be at least one year old and healed
-
No body glitter or lotions that have a strong smell
Students will participate in OSHA based blood borne pathogens training throughout the program. This will be verified prior to clinical assignment or labs. This training will be documented and documentation will be provided to the clinical sites upon request. BBP Training will initially be offered to each student during SUR1050 and must meet the course outcome requirement of 100%. Reinforcement of the BBP training will be incorporated into lab and other selected classes.
Prior to Surgical Observation days, students may be required to review the training by a stated deadline in order to participate. The test may be repeated one time only.
Sharps Injuries
Sharp injuries, although primarily accidental and preventable, are also inevitable in the operating room setting. If a student sustains some type of sharps injury while in the lab or clinical rotation, they are to:
-
STOP what they are doing
-
Isolate the injured anatomical part and the object that caused the injury
-
Notify their preceptor or instructor immediately of the break in technique and injury
-
Take themselves out of the picture once their preceptor or instructor steps in their place
-
Flush the injury with an antiseptic solution such as Betadine, alcohol, etc.
-
Notify the charge nurse or program director of the injury and follow their protocol for sharps injuries. What department the institution has the student go to in order to follow protocol varies from hospital to hospital, but may be any of the following
-
Employee Health/Occupational Health
-
Emergency Room
-
Off-site at an Employee Health Service
-
Or the student may see their own personal physician if none of these options are available
-
Obtain a copy of the facility’s incident report
-
Inform the Program Director of injury
-
Fill out a Baker College incident report next class session or email report of incident Baker College Incident Report Form Coming Soon!
Latex Allergies
As a concern for the safety and wellbeing of our students it is suggested that those individuals with a suspected or known Latex allergy understand the precautions to take for exposure. Students may require documentation of allergy testing confirming the extent of the allergy for accommodations. Because latex exposure in the surgical setting is unavoidable, it may be impossible for the student to be able to complete the clinical portion of this program; thus, resulting in the inability to complete a degree in Surgical Technology. Only Emergency Departments (ED’s) in Michigan are required to provide a Latex-free environment. Surgical Technology Labs and experience day areas may have Latex products present.
Pregnancy
As a participant in the Surgical Technology program at Baker College, you may be exposed to hazardous materials and infectious diseases and perform activities that pose a risk to your health and well-being. Additionally, due to the physical demands of the program, it may not be safe for you to continue your participation if you are pregnant. The potential risks and hazards of working in the perioperative services environment include, but are not limited to:
-
Radiation exposure: Radiation from X-rays and other imaging equipment used in the operating room can harm a developing fetus.
-
Anesthesia: Anesthetic drugs can cross the placenta and affect the fetus, leading to potential complications.
-
Infection: Operating rooms are high-risk areas for infection, and a pregnant woman working in an operating room may be at greater risk of infection, which can be dangerous for both the woman and her fetus.
-
Physical strain: Pregnant women may be at increased risk of physical strain due to the increased weight and size of their uterus, as well as changes in their center of gravity.
-
Exposure to hazardous materials: Operating rooms often contain hazardous materials such as chemicals (polymethylmethacrylate), sharps, and medical waste, which can pose a risk to a developing fetus.
-
Stress: The high-pressure, fast-paced environment of the operating room can cause stress, which can be harmful to a developing fetus.
Although it is not required, in order to protect the health of you and your unborn child, we recommend disclosing your pregnancy in writing, as soon as possible to the Program Director and/or the Clinical Coordinator. The voluntary disclosure of pregnancy to the Program requires:
If the student requests to inform the clinical site, the student must provide documentation to the program in regard to who was informed, the role of the person and a signed acknowledgement from the OR educator or Manager of the pregnancy. The clinical site does have the right to remove the student from the site. However, Baker College will try to place the student in another clinical site location. In the event another clinical location is unable to be secured, the student will be withdrawn from the program and allowed to return during the subsequent clinical semester without penalty. Failure on the part of the student to notify a program official, in writing, of an existing pregnancy shall absolve both the College and the clinical education center of any responsibility from an assignment to a potentially hazardous environment.
Professional Requirements and Technical Skills
These technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the program at Baker College. These standards are not conditions of admission to the program. Persons interested in applying for admission to the program should review this information to develop a better understanding of the physical abilities and behavioral characteristics necessary to successfully complete the program. The College complies with the requirements and spirit of Section 504 of the Rehabilitation Act and the Americans with Disabilities Act of 1990.
Therefore, the College will endeavor to make reasonable accommodations for participants with disabilities who are otherwise qualified. Safely access, prepare, and operate equipment and supplies in a variety of settings.
Affective Domain (Attitude)
-
Effectively communicate with classmates, faculty, and members of the surgical team when visualization of mouth/lips is restricted.
-
Demonstrate positive interpersonal skills during interactions with patients, staff, faculty and health care team members.
-
Demonstrate appropriate professional and procedural judgment decisions under stressful and/or emergency conditions (i.e. unstable patient condition), emergent demands (i.e. stat test orders), and a distracting environment (i.e., high noise levels, complex visual stimuli).
Cognitive Domain (Knowledge)
-
Access information from books, reference manuals, computers, and paper and electronic medical documents to accurately perform duties and safely use equipment.
-
Prioritize, organize, and utilize time-management skills to perform tasks such as, but not limited to, appropriately tracking surgical supplies and performing anticipation skills intraoperatively.
-
Respond appropriately to activation/warning signals on equipment.
-
Detect and respond appropriately to odors in order to maintain environmental safety and patient needs.
-
Recognize potentially hazardous materials, equipment, and situations and proceed safely in order to minimize risk of injury to patients, self, and nearby individuals by referencing, utilizing and adhering to OSHA requirements such as SMS (Material Safety Sheets) and standard precautions.
Psychomotor Domain (Skills)
-
Safely access, prepare, and operate equipment and supplies in a variety of settings.
-
Assist with transport and transfer of patient and equipment being able to lift 25-40lb equipment and instrument trays.
-
Assist with surgical procedures for prolonged periods without nourishment or restroom breaks.
-
Safely perform tasks such as, loading a fine (10-0) suture onto needles and needle holders while wearing safety glasses which requires fine motor control with corresponding hand-eye coordination.
-
Utilize instruments, supplies, and equipment safely within the operating suite.
-
Perform or assist with and/or transfer, lift, move, position, and manipulate the client who is unconscious.
Code of Ethics
Association of Surgical Technologists - Code of Ethics
-
To maintain the highest standards of professional conduct and patient care.
-
To hold in confidence with respect to the patient’s beliefs, all personal matters.
-
To respect and protect the patient’s legal and moral rights to quality patient care.
-
To not knowingly cause injury or any injustice to those entrusted to our care.
-
To work with fellow technologists and other professional health groups to promote harmony and unity for better patient care.
-
To always follow the principles of asepsis.
-
To maintain a high degree of efficiency through continuing education.
-
To maintain and practice surgical technology willingly, with pride and dignity.
-
To report any unethical conduct or practice to the proper authority.
-
To adhere to the Code of Ethics at all times in relationship to all members of the health care team.
Supervision Requirements
-
The student shall be supervised at all times by program officials when sharps are in use in the lab
-
The student shall be supervised by hospital personnel/designated preceptors at all times when in the clinical setting
-
All student activities within the clinical setting will be educational in nature.
-
Students will not be substituted for hired staff personnel within the clinical institution, in the capacity of a surgical technologist.
-
Program officials will maintain contact with students through regular clinical observation, email and phone calls.
Certification of Eligibility
Students who graduate from the Baker College Surgical Technology Program are eligible to take the National Certification Examination through NBSTSA. Passing the national examination qualifies the individual as a Certified Surgical Technologist (CST®).
Web Based Testing/Certification Exam
Baker College Surgical Technology Program participates in NBSTSA’s WBT (Web Based Testing). Arrangements are made for current surgical technology students to sit for the National Certification Exam prior or just after graduation. This exam is administered by an approved AMP proctor with no Health Science Affiliation. The NBSTSA web-based exam cost is included in the AST Gold Package. Students will participate in the exam as a component of the SUR 2590 course.
Curriculum Design - Sequencing of Courses
Requirements for Graduation
Competency Evaluation Framework
The Surgical Technology program utilizes the Miller’s Pyramid of clinical competency to evaluate students’ achievement of skill acquisition. This framework is used in medical/allied health education to assess levels of competency in clinical skills. It consists of four levels:
-
Knows
-
Knows How
-
Shows How
-
Does
During competency evaluation students are expected to score in the “Knows How” category to pass the competency exam. Students who score below this benchmark will be instructed to attend open labs and will be retested on the competency in one week.
Required Lab Competencies
SUR 2210 and SUR 2220 are the lab courses associated with the Surgical Technology program. Students are required to obtain a passing score on all competencies within these lab courses in order to progress in or graduate from the program and be eligible to sit for the certification exam. The final grade required in all surgical technology courses is (B-).
Students must meet two criteria to pass the lab courses:
A) 800 points or more as a final grade (i.e. B- in the course)
B) Obtain a passing score on the lab practical.
The lab competencies students are evaluated on include the following:
|
SUR 2210 - Surgical Technology Lab I
|
SUR 2220 - Surgical Technology Lab II
|
-
Anatomy of an instrument
-
Assemble an instrument set
-
Package items for sterilization
-
Operate a steam sterilizer
-
Avagard Application
-
Understanding operating room attire
-
Perform a medical handwash
-
Organize the OR
-
Read a surgeon preference card
-
Open back table pack and basin
-
Aseptically open instruments and supplies
-
Perform a surgical hand scrub
-
Don sterile gown and gloves
-
Drape a mayo stand
-
Gown and glove another team member
-
Remove soiled gown and gloves
|
-
Blood pressure assessment
-
Radial pulse assessment
-
Application of patient monitoring equipment
-
Patient transport and transfer to the OR Table
-
Specimen care
-
Patient and case clean up
-
Case preparation
-
Open gloving
-
Patient positioning and padding
-
Patient skin prep
-
Establish a sterile field
-
Perform an Avagard scrub
-
Don gown and gloves
-
Organize supplies on the back table
-
Accept and handle medications
-
Drape a mayo stand
-
Gown and glove a team member
-
Drape the patient
-
Initiate time out
-
Handle and pass sharps
-
Handle suture ties
-
Surgical counts
-
End of procedure duties
|
Competency Failure
Definition of competency failure
Competency failure is defined as the inability of a student to meet the established criteria for proficiency in a specific skill or procedure during a competency assessment.
Notification of Competency Failure
The instructor or clinical preceptor will provide the student with timely and constructive feedback regarding areas of deficiency and the specific criteria that were not met.
Opportunity for Competency Retake
-
Students who fail to demonstrate competency in a particular skill or procedure will be provided with the opportunity to retake the competency assessment
-
Retakes are scheduled one week after the initial assessment and at the discretion of the program faculty.
-
Retakes will be scheduled outside of the regular course time to accommodate lab course schedules
Competency Retake Procedures
During the retake, students will be evaluated based on the same criteria and standards used in the initial assessment. If the student is unable to complete the required skill or procedure they will be administratively withdrawn from the Surgical Technology program and will need to follow the application process for readmittance. If the student is unable to complete the required skill or procedure they will be administratively withdrawn from the Surgical Technology program and will need to follow the application process for readmittance.
Clinical Course Information
SUR 2510 and SUR 2520 are clinical courses associated with the Surgical Technology Program. The clinical component of the Surgical Technology program is rigorous and requires students to spend up to 40 hours in the clinical setting for the duration of the Spring semester (16 weeks). Clinical shifts require students to be at their clinical site for a minimum of 8 hours per clinic day and up to four days per week. Variations of this schedule will need prior approval by the clinical site and Baker College clinical coordinator or program director.
CLINICAL PLACEMENT
Each clinical internship course requires the students to complete a minimum of 240 to a maximum of 256 clinical hours per site.
Clinical Placement Policy
-
Clinical sites are located throughout the state of Michigan and may require variable commute distances from their home campus location.
-
Students will be notified of their clinical placement during week 10 of the semester preceding clinical rotations.
-
Clinical placements are based on the home address of the campus, rather than the student’s individual address.
-
Clinical placements are determined by the Surgical Technology Program Director and/or Clinical Coordinator
-
Every effort will be made to accommodate student preferences regarding clinical placements, but final placements are subject to availability and program/case requirements.
-
Requests for placement adjustments due to extenuating circumstances will be considered on a case-by-case basis.
Clinical Attendance
-
If the student refuses the assigned clinical placement, the College is not obligated to seek an alternative placement.
-
Reliable transportation is a requirement for all scheduled class and clinical obligations.
-
Because of the variety of surgical cases students must participate in, students may be rotated through more than one clinical site during their clinical rotations. Students who decline to go to alternative clinical sites risk not meeting clinical case requirements which would result in an Incomplete in the clinical component of the program, preclude the student from sitting for the Certifying Surgical Technologist Exam, and therefore not meet the requirements for graduation.
-
Students who are removed from a clinical site due to violations of hospital or college policies will automatically fail the clinical course and face other disciplinary action.
-
Students are expected to be at their clinical site a minimum of 15 minutes prior to the start of their clinical shift to allow time to change into the required clinical attire and make it to their assigned operating room 30 minutes prior to the patient arrival.
-
Tardiness to clinical sites is not acceptable. Tardiness to the clinical site is defined as not being in the assigned operating room 30 minutes before the scheduled start of a surgical case. If a student is late to their clinical site more than twice, they will be placed on a Learning Contract. Future late arrivals will result in dismissal from the Surgical Technology Program.
-
Students must notify the Program Director or Clinical Coordinator if they are staying past their normal clinical hours.
-
Students may participate in “on-call” shifts but only with the advanced notice and permission of the Clinical Coordinator or Program Director.
Absence from Clinical
-
Attendance at your clinical site during assigned clinical hours is mandatory. Failure to meet the minimum hour requirement during a clinical rotation will result in the student receiving an Incomplete grade and inability to move to the next clinical site, sit for the Certification Exam and/or meet the requirements for graduation.
-
If a student needs to leave their clinical site early for any reason, they must follow the policies of the clinical site and inform the Program Director and Clinical Coordinator.
Procedure for Reporting and Absence
-
Unplanned Absence: If a student is absent from a clinical site for any reason, the student must notify the site by telephone as well as the Program Director and Clinical Coordinator no less than 30 minutes prior to the start of the clinical shift and provide documentation as to who they spoke with at the clinical site.
-
Planned Absence: If a student is aware of a planned absence, they must work with the clinical site, the Program Director, and the Clinical Coordinator to make up the hours missed.
-
Students are allowed to miss up to 16 hours OR 2 days of clinical time for personal reasons. These missed hours or days must be approved and documented by the Program Director and/or the Clinical Coordinator. Documentation must be provided by the student to the Program Director and Clinical Coordinator proving the student informed their clinical site of a planned absence.
-
If the student misses more than 2 days of clinical, the student will be placed on a learning contract for the duration of the semester. Any missed clinical time above 2 missed days or 16 hours may result in an incomplete in the clinical course and the student will be required to make up the missed time.
-
If the Program Director or Clinical Coordinator is made aware of an undocumented student absence, the student will be placed on a Learning Contract and any further violation of the attendance policy will result in dismissal from the Surgical Technology program.
-
In the event your Baker College campus closes (power outage, weather, etc.) the student will still report to their clinical site unless specifically instructed by the Program Director or Clinical Coordinator. If travel conditions are deemed unsafe, the student must inform the Program Director and Clinical Coordinator and a plan will be made to make up the clinical hours.
-
BC is unable to find additional clinical placements for students who are removed from clinicals due to unprofessional behaviors and/or at the request of the clinical site. The Program Director and Dean will review clinical placement requests for extenuating circumstances.
Clinical Hour Make-Up Policy
Students must make every attempt to obtain all required clinical hours in the clinic setting. However, in the event a student must leave early or is absent from clinical a maximum of 16 missed hours can be made up through the following measures:
-
Staying later during scheduled clinical days. The student may stay at the clinical site for more than 8 hours with the permission of the clinical site and the program director or clinical coordinator. The program director, student and clinical site will schedule the make up hours as necessary.
-
Case studies. The student may submit a written clinical case study for a surgical case that will be assigned by the program director or the clinical coordinator. The case study must be a minimum of 5 pages, follow all APA requirements and be written in a scholarly manner. Each case study will be worth 4 hours of clinical time. A maximum of 2 case studies is allowed per student.
-
AST Continuing Education Journal Article summary and exam. Students may submit up to 8 CEUs from AST continuing education journal articles for a total of 8 clinical hours. The student must submit a 1 page summary of the article (in APA format) and a screenshot of the passing score of the post article exam.
The route of clinical make up hours must be approved by the program director or clinical coordinator prior to submission and the student will be placed on a learning contract. Failure to meet minimum clinical hours will result in an Incomplete grade for the clinical rotation until the hours are completed.
Clinical Surgical Case Requirements - Counting Cases
Case Requirements - A student must complete a minimum of 120 cases as delineated below:
-
General Surgery
-
A student must complete a minimum of 30 cases in General Surgery.
-
20 of these cases must be performed in the First Scrub (FS) role
-
The remaining 10 cases may be performed in either the FS or SS role.
-
Specialty Surgery
-
A student must complete a minimum of 90 cases in various surgical specialties, excluding General Surgery.
-
A minimum of 60 cases must be performed in the FS role and distributed amongst a minimum of four surgical specialties
-
a minimum of 10 cases in four different specialties must be completed in the FS role
-
The additional 20 cases in the FS role may be distributed amongst any one surgical specialty or multiple surgical specialties.
-
The remaining 30 cases may be performed in any surgical specialty in either the FS or SS role.
-
Surgical specialties (excluding general surgery)
-
cardiothoracic
-
genitourinary
-
neurologic
-
obstetric and gynecologic
-
orthopedic
-
otorhinolaryngologic
-
ophthalmologic
-
oral/maxillofacial
-
peripheral vascular
-
plastics and reconstructive
-
procurement and transplant
-
Counting cases
-
cases may be counted according to surgical specialty as defined by the core curriculum
-
one pathology is counted as one procedure
-
breast biopsy followed by mastectomy - one procedure
-
counting more than one case on the same patient
-
a procedure that requires different set-ups and includes different specialties may be counted as two separate cases. A mastectomy procedure followed by immediate reconstruction or augmentation are counted as separate cases.
-
Diagnostic vs. operative endoscopy cases
-
an endoscopy classified as a semi-critical procedure is considered a diagnostic case
-
An endoscopy classified as a critical procedure is classified as an operative case
-
Diagnostic and operative cases will be counted according to specialty.
-
Diagnostic cases are counted in the SS role up to a total of 10 of the 120 cases
-
example: a cystoscopy is a diagnostic procedure. If an adjunct procedure is performed (such as the placement of a stent) it is an operative procedure.
-
vaginal delivery cases are counted in the SS role of the OB/GYN specialty, up to a total of five of the required 120.
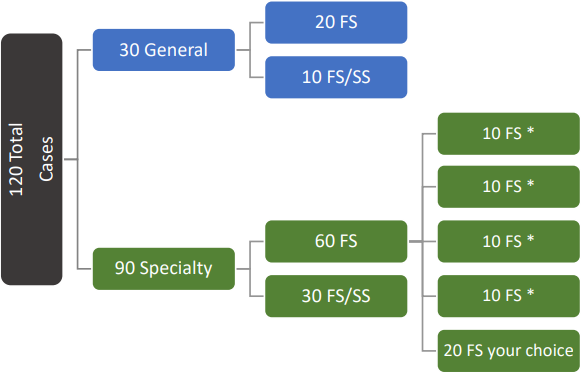
First Scrub Role
The student surgical technologist shall perform the following duties during any given procedure with proficiency. The student must meet the following five criteria to count the case in the First Scrub Role:
-
Verify Supplies and Equipment needed for the surgical procedure
-
Set up the sterile field with instruments, supplies, equipment, medication(s) and solutions needed for the procedure
-
Perform counts with the circulator prior to the procedure and before the incision is closed
-
Pass instruments and supplies to the sterile surgical team members during the procedure
-
Maintain sterile technique as measured by recognized breaks in technique and demonstrate knowledge of how to correct with appropriate technique
Second Scrub Role
The student who is at the sterile field who has not met all criteria for the first scrub role, but actively participates in the surgical procedure in its entirety by completing any of the following:
Observation Role
The observation role is defined as the student who is in the operating room performing roles that do not meet the criteria for the first or second scrub role. These observation cases are not to be included in the required case count, but must be documented by the program.
Required Clinical Case Documentation:
-
case performed
-
role performed
-
performance evaluations
-
weekly preceptor
-
clinical coordinator
Documentation of clinical cases and roles performed must be validated by a clinical and preceptor and verified by the program director or clinical coordinator.
Clinical Competencies
Required Clinical Documentation
Students will be required to submit weekly clinical documentation and paperwork describing the cases and roles they performed and the hours spent in their clinical site. This documentation is an accreditation required artifact of learning. Any instance of falsified documentation will result in immediate dismissal from the Surgical Technology program.
Re-Entry Into the Surgical Technology Program
Students who leave the program, for reasons other than noncompliance with policies and procedures, may be able to apply for readmission one time. The readmission of students is at the discretion of the Dean of Health Sciences, Director of Surgical Technology Programs and any other student advocate Baker College personnel. Re-entry may be dependent on class size and clinical site availability. Students must submit, in writing, their request for re-entry by a designated date set by Baker College personnel.
If it has been more than one year since the student has taken Surgical technology major courses, the Program Director may set specific conditions necessary to bring the student to the proper level of competency prior to re-entry. This may include the need to audit or retake previous courses and/or demonstrate knowledge and competency in regards to their didactic and clinical skills.
Clinical Work Policy
Baker College Surgical Technology students are allowed to be compensated for hours worked in the clinical environment. However, to ensure that students receive appropriate supervision and education in accordance with industry and educational standards, the following policies and procedures must be followed.
Responsibilities of the Clinical Site
-
Notify the surgical technology program director of the intent to “hire” the surgical technology student.
-
Provide a comprehensive job description for the position.
-
The job description must state the student is not a paid employee but rather an intern gaining practical experience as part of their educational program.
-
Never substitute the surgical technology student as a paid staff member
-
The student must be always under the direct supervision of a surgical technology preceptor.
-
Provide a qualified surgical technologist preceptor.
-
The preceptor must be employed by the clinical affiliate.
-
The preceptor must be a Certified Surgical Technologist (CST) or be eligible for certification through the National Board of Surgical Technology and Surgical Assisting (NBSTSA).
-
Sign a contract attesting to the above-named responsibilities of the clinical site.
Responsibilities of the Surgical Technology Clinical Student
-
Notify the program director and/or clinical coordinator of the intent to enter into an employment contract with the clinical site.
-
Never work alone in the role as “Surgical Technologist” while still enrolled in the Baker College Surgical Technology program.
-
Promptly notify the program director or clinical coordinator of instances where the student was substituted for staff or left unsupervised in the role of surgical technologist.
-
Sign a contract attesting to the above-listed requirements.
Any violation or omission of the above listed policies will result in all clinical hours and cases accrued by the student at the clinical site to be voided.
VETERINARY TECHNOLOGY
Program Overview
A veterinary technician can best be thought of as an animal nurse. By definition, a veterinary technician is a person who has completed a 2-year associate degree in Veterinary Technology from an AVMA (American Veterinary Medical Association) accredited institution. The Veterinary Practice Act of Michigan allows veterinary technicians to do anything for the care of animals except diagnose disease, prescribe medication and perform surgery. Besides providing nursing care, veterinary technicians also function as laboratory technicians, radiology technicians, pharmacy technicians, surgical technicians and anesthesia technicians. In addition, veterinary technicians are often responsible for a majority of the client education that occurs in a veterinary practice; thus, this is a profession that requires excellent communication skills.
The veterinary technology profession is very diverse and the opportunities for technicians are extremely varied. Career opportunities exist within, but are not limited to the following areas: small animal hospitals, large animal hospitals, research, education, pharmaceuticals, public health, federal and state government and the military. Once a student has successfully graduated from an AVMA accredited program, he/she can sit for the national licensing exam. If the graduate passes the VTNE exam, he/she will be eligible for licensure as a Licensed Veterinary Technician (LVT) in the state of Michigan.
Accreditation Information
Accreditation is granted through the American Veterinary Medical Association, Committee on Veterinary Technician Education and Activities (AVMA, CVTEA). Cadillac, Jackson and Muskegon are currently accredited.
American Veterinary Medical Association, Committee on Veterinary Technician Education and Activities (AVMA, CVTEA)
1931 North Meacham Road, Suite 100, Schaumburg, IL 60173-4630
(800) 248-2862; fax: (847) 925-1329
The Higher Learning Commission
230 South LaSalle St., Suite 7-500, Chicago, IL 60604-1411
(800) 621-7440
State and National Organizations
Students are strongly encouraged to become actively involved in professional associations. Student membership is available to Baker College Veterinary Technology students at a reduced rate for both the National Association for Veterinary Technicians of America (NAVTA) and the Michigan Association of Veterinary Technicians (MAVT). They provide continuing education that meets state licensing requirements, maintain relations with the organizations responsible for the testing and credentialing of technicians, offer a support network for technicians and provide a wealth of information and resources.
● NAVTA National Association of Veterinary Technicians in America
● MAVT Michigan Association of Veterinary Technicians
Goals
- To prepare students for competency in the knowledge of animal health and veterinary issues.
- To prepare students to confidently and effectively perform the essential skills and tasks commonly encountered in veterinary facilities.
- To provide general education that expands students’ horizons, develops strong communication skills and encourages critical thinking.
- To encourage social and classroom related activities, which promote both personal and professional growth.
- To assist graduates throughout their careers in securing employment and improving career opportunities.
- To promote the image and prestige of the veterinary technician profession by encouraging professional behavior and community service.
Mission
The mission of the Veterinary Technology program at Baker College is to provide both didactic and clinical education to prepare students to enter and enhance the veterinary healthcare team and the competent care of animals by providing a skill set that includes clinical proficiency, critical thinking and strong communication.
Program Outcomes/Philosophy
By the end of the program, students will:
- Apply knowledge of global practices, scientific practice, medical terminology, anatomy and physiology, pathophysiology and disease processes within veterinary medicine.
- Communicate in all formats, written, oral, nonverbal and electronic, with a diverse client population, other health care team members and the public in a professional and effective manner.
- Apply ethical standards and federal and state regulatory guidelines in the veterinary setting.
- Properly classify medications commonly used in veterinary medicine.
- Properly calculate and administer the appropriate dose of ordered medications.
- Apply proper, safe radiological procedures within the veterinary laboratory setting.
- Perform appropriate, effective and efficient diagnostic laboratory procedures within the veterinary laboratory setting.
- Perform proper nursing procedures within a veterinary setting.
- Successfully administer surgical assistance, postoperative care, anesthesia and dentistry within a veterinary setting.
- Utilize safety and health regulations and policies on the care and use of laboratory animals, husbandry, care and treatment and the importance to the environment while selecting or procuring exotic animals and animals used in research.
- Prepare to take the national licensing exam.
Code of Ethics
Students will adhere to the Personal and Professional Conduct policies found in the Baker College Student Handbook.
Code of Ethics of the National Association of Veterinary Technicians in American (NAVTA):
Veterinary technicians shall aid society and animals through providing excellent care and services for animals.
- Veterinary technicians shall prevent and relieve the suffering of animals.
- Veterinary technicians shall promote public health by assisting with the control of zoonotic diseases and informing the public about these diseases.
- Veterinary technicians shall assume accountability for individual professional actions and judgments.
- Veterinary technicians shall protect confidential information provided by clients.
- Veterinary technicians shall safeguard the public and the professional against individuals deficient in professional competence or ethics.
- Veterinary technicians shall assist with efforts to ensure conditions of employment consistent with the excellent care for animals.
- Veterinary technicians shall remain competent in veterinary technology through commitment to life-long learning.
- Veterinary technicians shall collaborate with members of the veterinary medical profession in efforts to ensure quality health care services for all animals.
Safety Requirements
The following information is to ensure awareness by the student of the unique circumstances, requirements and potential hazards related to the course of study of Veterinary Technology. Baker College attempts to offer the most modern teaching methods and curriculum coupled with a most extensive practical, hands-on externship experience in contemporary Veterinary Medical practice. By the nature of the involvement with live animals and clinical facilities there are some circumstances, requirements and potential hazards inherent in this program. All students should fully understand these situations and requirements and be able to make an informed decision to continue in the program.
Exposure to Hazards
- Live Animals: Students will be exposed to live animals. At times there will be the potential of injury by small or large animals during the course of their treatment.
- Zoonotic Diseases: Zoonotic diseases are those diseases that can be transmitted from animals to humans. Students will be exposed to sick animal patients. All due diligence will be paid to ensure that the possibility of transmission of zoonotic diseases from patients to students and staff will be held at a minimum. Students must be aware that they will be at potential risk for contracting diseases from their patients. Information on specific disease risks will be promulgated on a case-by-case basis as needed. Specific questions should be directed to the Veterinary Technology Program Director.
- Exposure to ionizing radiation: The use of diagnostic X-ray is a component of contemporary veterinary practice. During the course of clinical practice students will be exposed to ionizing radiation from x-ray equipment. Proper shielding and dosimetry will be provided to all students prior to exposure.
- During VET courses, required competencies of diagnostic and treatment techniques subject students to radiation.
- To abide by the Occupational Safety and Health Association (OSHA) guidelines, the program monitors the level of exposure to each student registered for a VET course.
- Badges are distributed by program personnel.
- Each student is responsible for this badge at all times after distribution by program personnel.
- All radiology badges must be turned in to the Program Director as scheduled. The student will receive a schedule.
- The badges will be sent in for a recording of the radiation exposure of each student. Lost radiology badges will incur a $20 replacement fee on the student.
- As mentioned in the section on dress code, radiology badges must be present with the student at all laboratory and externship activities. The student must wear the radiology badge for EVERY activity involving radiation. Failure to do so will result in student dismissal from that activity, which may affect the student’s overall grade and competency for that required task.
- All documentation of student radiation exposure will be placed in the student’s program health file.
- Exposure to Hazardous Materials: Students will be exposed to a variety of materials and some of which are potentially hazardous to human health. Students will always have access to Material Safety Data sheets on any and all potentially hazardous materials. Students and staff will comply with all safety and protective equipment regulations, outlined by the Occupational Safety and Health Administration and the Michigan Occupational Safety and Health Administration, when handling potentially hazardous materials.
Rabies Immunization Protocol
The AVMA Committee on Veterinary Technician Education and Activities (CVTEA)® has released a publication of the Accreditation Policies and Procedures (P&P) Manual of the AVMA CVTEA effective January 1, 2022. The Committee amended Standard 4e as follows:
Standard 4e. Safety of students, program personnel, and animals must be of prime consideration. Students must be educated on rabies risk prior to working with animals. Prior to live animal use, students must be vaccinated against rabies.
Therefore, all incoming Veterinary Technology students are required to complete Rabies Pre-exposure vaccination or provide proof of acceptable titer (if previously vaccinated) in order to progress through the program and be eligible to interact with live animals during required course lab activities, competencies, and participation in clinical/externship placement. Veterinary Technology students are expected to complete Pre-exposure Rabies vaccination series prior to animal handling. Students who have not provided verification of vaccination or acceptable titer will be required to follow the
mitigation plan developed by the college which may prohibit the student from completing all required skills necessary to matriculate from the program.
Students will be able to receive the rabies vaccination series either through their own health care provider (out-of-pocket student expense), through the county health department, or through local Walgreen or CVS pharmacies. Program directors can assist with providing specific links to resources. The cost of the vaccines will be financial aid eligible. Each student is responsible for contacting the financial aid department in order to apply this rabies immunization fee to their financial aid packet from Baker College. Failure to notify the financial aid office results in the student being personally responsible for payment of the immunizations.
Students are required to review the information regarding rabies from the Center for Disease Control (CDC) and the American Veterinary Medical Association (AVMA) websites.
Each student must complete the Baker College Health Immunization Form located on the Veterinary Technology Information page. A student signature is required on the Vaccination and Clinical Exposure Notice/Agreement Form All documents will be confidentially stored in the student’s program health file. Baker College Health Immunization Form Coming Soon!
Policy Concerning Temporarily Disabled, Potentially Pregnant and Pregnant Students
Potential for injury increases when an individual is pregnant or temporarily disabled due to any cause, such as injury or disease. An illness may also, for instance, leave a student with a compromised immune system. Because of the inherent risks to students and unborn children in veterinary medicine and the clinical and lab environments and the associated exercises that are endemic to the study of veterinary technology, all students must take responsibility for their own health status and those who are potentially pregnant, temporarily disabled or pregnant must take whatever added precautions necessary to safeguard health with the professional advice of their physician.
It is expected that an affected student will complete all requirements of the program as may be reasonably accommodated as necessary under the circumstances and as students may wish to assume the greater risks associated with participation when temporarily disabled or pregnant.
Upon voluntary reporting and confirmation of the pregnancy, students will:
- Complete and submit the “Notice of Pregnancy Form” to the Programs
- Clinical Coordinator and Clinical Supervisor.
- Submit a statement from a physician verifying pregnancy and expected due date. The statement must include the physician’s recommendation of the following options:
- Immediate leave of absence
- Withdrawal from clinical rotations with continued participation in
- Didactic instruction.
- Continued clinical rotation with no restrictions.
Students with temporary disabilities or who are pregnant will be asked to discuss potential harm with, and may be strongly advised by faculty against participation in any activity where the risk for accidents or exposure to hazards is too high. The student may appeal such a decision. Copies of all documents pertaining to a medical condition affecting a student’s assignment must be maintained in a confidential student’s file.
Options for Pregnant and Temporarily Disabled Students
- The student can voluntarily elect to participate in any clerical or observation portions of his or her classes or clinical experience. The student will receive an incomplete for the class/externship but will be allowed to finish clinical hours and class checklist when the student is no longer pregnant or temporarily disabled.
- The student can assume all risk to himself or herself and, if pregnant, the fetus, releasing Baker College and the Clinical Site and complete clinical experiences, including classes that include labs. Special arrangements will be made to fulfill the radiology requirement that will not involve any radiation exposure. The student must have a signed physician visit checklist.
- A pregnant or temporarily disabled student may voluntarily withdraw from the program. After the pregnancy and/or when the student is physically able, they will be readmitted as a student in the next class in the veterinary technology program. This option minimizes known risks.
Risks
Didactic portions of the program will inform students of the potential hazards and the safety and professional procedures that must be observed at all times. However, if a student is or becomes pregnant, temporarily disabled or immunosuppressive, that there are risks that may specifically pertain to the student and should be disclosed as potential concerns to their physician. In addition, there may even be unknown risks that could affect the student and/or an unborn child. The following list is illustrative and is not intended to be an exhaustive list. Any potentially pregnant, temporarily disabled, pregnant or immunosuppressed student may wish to have his or her physician contact the Program Director to discuss their particular situation and specific potential hazards and concerns.
- Exposure to anesthetic gasses (Isoflurane, Sevoflurane)
- Exposure to radiation.
- Exposure to teratogens, including cytotoxic compounds, chemical agents, sterilizing agents, cleaning agents, preserving agents and fixing agents
- Zoonotic diseases, including but not limited to:
- Rabies
- Leptospirosis
- Lyme Disease and other tick-borne diseases
- Giardia
- Visceral Larval Migrans
- Brucellosis
- Fungal diseases
- Toxoplasmosis
- Animal bites and their associated complications including but not limited to lympha denopathy, septicemia, death and disfigurement
- Manual labor - lifting of animals, dog food bags etc.
- Cat Scratches - exposure to Cytauxzoon felis (Cat Scratch Disease)
- Exposure to hormones (e.g., prostaglandins and progesterones)
- Kicks or other physical contact, especially from large animals.
The clinical site has final approval regarding placement of a student for externship. The clinical site can dismiss a student from a clinical site at any time with their discretion. If a clinical site does not provide approval, the College will make every reasonable effort to identify a site that will meet the requirements of the program. The College is responsible for identifying the clinical site.
Advanced Placement/Transfer Policy
The CVTEA recognizes that academic institutions have the inherent right to accept credits from other colleges, universities, recognized educational entities or prior learning. However, if the program accepts veterinary technician-related course credit from institutions not accredited by AVMA CVTEA, the program must ensure that the rigor of transfer courses meets CVTEA Standards. Provision of prior learning must include documentation or critical evaluation of these experiences to award college credit or advanced standing. Documentation of the assurance may be requested for review during the program accreditation process. At times, accredited programs are requested to give credit for high school courses with titles similar to those required for graduation from a CVTEA-accredited program. If credit is to be given for such courses, the student must first be required to demonstrate to the veterinary technology program faculty a level of competency comparable to that of students who complete the required course successfully.
Professional Requirements and Technical Skills
All Veterinary Technology Students are expected to dress in a professional manner. During the professional track of the curriculum, students will be required to wear program specific scrubs.
All students are required to have the following items during the laboratory procedures and externships:
- Student Photo ID badge
- Radiology Badge (supplied by the program)
- Calculator (four function only)
- Stethoscope
- Digital thermometer
- Black ink pens
- Small Notebook
- Watch with second hand
- Knee high waterproof boots
- Coveralls
Each program may have dress requirements that are specific for the off-campus large animal activities that will occur throughout the professional program. The student must check with the appropriate program personnel for required attire. Dress code for the clinical sites will be dictated by the hospital or facility policy. Students may be required to purchase clothing or uniforms required by a particular site. It is the responsibility of the student to arrive at the clinical site looking professional. White lab coats must be worn during laboratory sessions. All clothing and lab coats must be clean and presentable.
For safety and sterility purposes, no student will be allowed to wear any type of jewelry as a result of eyebrow piercing, nose piercing or tongue piercing to any laboratory, clinical site or externship. Hoop and dangle earrings are not permitted and only stud earrings will be allowed. Open-toed shoes, sandals, Crocs® and steeled-toed boots are not allowed; closed-toed shoes must be worn for both lecture and lab. In addition, all rings, watches, bracelets and earrings need to be removed prior to gloving into surgery.
Fingernails are to be natural, short, neatly maintained and unpolished when gloving into surgery. Hands are to be kept clean.
These technical standards reflect performance abilities and characteristics that are necessary to successfully complete the requirements of the program at Baker College. These standards are not conditions of admission to the program. Persons interested in applying for admission to the program should review this information to develop a better understanding of the physical abilities and behavioral characteristics necessary to successfully complete the program. The College complies with the requirements and spirit of Section 504 of the Rehabilitation Act and the Americans with Disabilities Act of 1990. Therefore, the College will endeavor to make reasonable accommodations for participants with disabilities who are otherwise qualified.
- Must be at least 18 years of age to operate diagnostic imaging equipment to comply with State of Michigan rules for radiation safety.
- Effectively communicate in English, both verbally and in writing (documentation) utilizing accurate and appropriate terminology with animals’ families/owners and members of the healthcare team in person or by telephone.
- Effectively communicate with others when visualization of mouth/lips is restricted such as in a surgical setting.
- Access information from books, reference manuals, computers and paper and electronic medical documents to accurately perform duties and safely use equipment.
- Auscultate body sounds, characterizes them and interprets findings appropriately.
- Recognize and respond appropriately to distress sounds from animal and alarms/warning signals on animal monitoring equipment directly and through intercommunication systems to ensure patient safety.
- Detect and respond appropriately to odors in order to maintain environmental safety and patient needs.
- Accurately palpate and interpret findings, i.e., palpation of pulses, lymph nodes or trachea to determine proper endotracheal tube size.
- Accurately observe variations in skin color, integrity, pulsations, tissue swelling, etc.
- Observe/guard and respond appropriately to animals’ response before, during and after treatment.
- Accurately characterize and interpret the color, odor, clarity and viscosity of body structures and fluids.
- Obtain optimum quality of radiographic images and correctly interpret an ECG tracings recorded in shades of gray.
- Safely perform tasks such as loading a fine (5-0) suture onto needles while wearing safety glasses that require fine motor control with corresponding hand-eye coordination.
- Accurately assesses equipment, medication, solutions and other products/supplies to ensure animal safety.
- Accurately interpret and validate text, numbers and graphs from print and video monitors.
- Evaluate, synthesize and communicate diagnostic information to the attending veterinarian.
- Recognize and correct performance deviations.
- Safely access, prepare supplies and instruments and operate equipment in a variety of indoor settings (i.e., intraoperative, ICU, examination areas) and outdoor settings such as a farm field or barn.
- Prioritize, organize and utilize time-management skills to perform tasks.
- Perform or assist with transfer, lifting and positioning of large and small animals.
- Demonstrate appropriate professional and procedural judgment decisions under stressful and/or emergency conditions (i.e., unstable patient condition), emergent demands (i.e., stat test orders) and a distracting environment (i.e., high noise levels, complex visual stimuli, aggressive animals).
- Recognize potentially hazardous materials, equipment and situations and proceed safely in order to minimize risk of injury to animals, self and nearby individuals by referencing, utilizing and adhering to OSHA requirements such as SDS (Safety Data Sheets) and universal precautions.
- Adhere to HIPAA, professional guidelines and code of ethics, Baker College conduct guidelines and clinical and externship sites’ policies and procedures.
Supervision Requirements
The veterinary technician’s role is to provide professional health care in conjunction with the veterinarian. The duties of veterinary technicians shall be performed under the direction, supervision and responsibility of veterinarians. These duties shall be accomplished in compliance with federal, state and local laws. These duties shall not include diagnosing, prescribing or performing surgery except where explicitly permitted by regulation.
An appropriate program personnel-to-student ratio must be maintained to ensure student safety and adequate delivery of instruction in program specific courses. Program personnel to student ratios shall not exceed 1:12 for laboratory courses without animals present and 1:8 for laboratory courses with animals present.
Successful completion of all required skills found in the Veterinary Technology Student Essential and Recommended Skills List, Appendix I must be evaluated and documented, indicating date completed, by program personnel who use standard criteria that reflect contemporary veterinary practice. Program personnel evaluating skills should be a veterinarian or a credentialed veterinary technician who is a graduate of an AVMA CVTEA or CVMA-accredited veterinary technology program.
Licensure Requirements
The AAVSB American Association of Veterinary State Boards owns and delivers the Veterinary Technician National Examination (VTNE). Most states and provinces use the VTNE to evaluate the competency of entry-level veterinary technicians and require a passing score on the VTNE in order for a veterinary technician to be credentialed.
Beginning with the July/August 2019 administration windows, the American Association of Veterinary State Boards (AAVSB) will review and determine Veterinary Technician National Examination (VTNE) eligibility for all Michigan candidates. Applicants must have graduated from an American Veterinary Medical Association (AVMA) approved veterinary technician educational program.
An applicant for a Michigan Veterinary Technician License must apply to the Michigan Bureau of Licensing and Regulatory Affairs upon achieving a passing score on the VTNE.
Curriculum Design - Sequencing of Courses
Competencies
Successful completion of all required skills found in the Veterinary Technology Student Essential and Recommended Skills List,
Appendix G must be evaluated and documented, indicating date completed, by program personnel who use standard criteria that reflect contemporary veterinary practice.
Clinical Hours
Each student must complete a minimum of 240 hours of clinical experience. Students will be assigned to clinical sites at the sole discretion of the program director or clinical coordinator. These internship experiences are to be unpaid. Additional internship hours may be required to complete necessary competencies.